https://hbr-org.cdn.ampproject.org/v/s/hbr.org/amp/2021/07/staying-visible-when-your-team-is-in-the-office-but-youre-wfh?amp_gsa=1&_js_v=a6&usqp=mq331AQIKAGwASCAAgM%3D#amp_tf=From%20%251%24s&aoh=16277387182512&csi=0&referrer=https%3A%2F%2Fwww.google.com&share=https%3A%2F%2Fhbr.org%2F2021%2F07%2Fstaying-visible-when-your-team-is-in-the-office-but-youre-wfh
Category: Beating Depression
5 Emotions You Didn’t Know Were Part of Grief
Disillusionment during the grief process.
Posted June 24, 2021 Reviewed by Kaja Perina
Key points
- Our understanding of grief fails to include many common emotional experiences.
- Grief can include guilt, numbness, disillusionment, relief, and gratitude.
- Naming our experiences as part of grief helps us grieve better.
Many people’s frame of reference for grief comes from Elisabeth Kübler-Ross’ five stages of grief. In her analysis, a grieving person will move through denial, anger, depression, bargaining, and acceptance. And while all of these may be part of the grief experience, the simplified description of these phrases fails to chart the wide emotional range of experiences a grieving person may experience. Here are some other emotional experiences a grieving person may encounter.
1. Guilt
Many struggle with guilt in the aftermath of a loss. Some feel guilty that their loved one died while they survived; others grapple with things said in anger or left unsaid. They may fixate on their most unflattering moments with the person lost rather than thinking about the relationship as a whole. When a person dies, sometimes a person will brush over a nuanced relationship with broad strokes, creating a distorted picture of reality. In addition to death, when grieving a lost job, opportunity, or relationship, a person may feel guilty for things said, unsaid, done, not done, done poorly, or done well but not soon enough to prevent the loss. Guilt after a death or other loss can lead to rumination at what could have or should have been,
2. Numbness
While not an emotion per se, numbness describes the lack of feeling that may come over a person in grief. That absence may feel alarming, but numbness is the mind’s way of protecting a person from feeling overloaded. We simply cannot sit in a constant state of overwhelming pain and so the mind responds with periods of numbness. Kubler Ross may aptly file this under the heading of denial, but the details are worth describing. Some may worry that numbness means something about their feelings about their loved one’s death. Not so. While less intense grief may speak to feeling ok with the loss, numbness can be a feature of profound sadness.
3. Disillusionment
When a person suffers a loss, they may become profoundly disillusioned with the world around them. Most commonly discussed is the loss of faith in God in the face of a loved one’s suffering, but it may take other forms. A person may feel disillusioned by the medical establishment after a difficult hospital experience. They may feel disillusioned by their family or community if they felt unsupported or abandoned during their time of need. Disillusionment can set a person emotionally adrift, feeling unable to count on the institutions and people that helped them feel grounded.
4. Relief
After a loss, a mourner may sigh in relief that the ordeal is over. Whether that ordeal is a death after a long illness, the end of tumultuous relationship, or a lost friendship, the lead up to the ending can be profoundly depleting. Many begin mourning before the loss even occurs (a phenomenon called anticipatory grief). When all is said and done, when money is drained, energy expended, and hope depleted, the person may feel glad that the loss has finally occurred and the process of healing and moving forward can finally commence.
5. Gratitude
As we make sense of the loss, some find gratitude in their grief. They may feel grateful for the time with the person lost, grateful for an opportunity they received, or grateful for what that lost thing gave them. Gratitude while grieving can occur fleetingly, intermittently, or in a sustained way. A person may feel resentment and anger one moment and gratitude the next. The key with gratitude is to accept it when it comes without forcing its hand, as sometimes happens with well-meaning loved ones in times of suffering.
Grief is a complicated, nuanced emotional experience that fluctuates, ebbs, and flows. The more nuance we can infuse into our collective understanding of grief by naming its component parts, the better we can honor our own experience and support loved ones going through it.
A Video Of A Guy Explaining An Easy Yet Brilliant Way To Make Friends As An Adult Went Viral With Almost 6M Views | Bored Panda
7 Downsides of Hope
https://www.psychologytoday.com/ca/blog/evolution-the-self/201807/7-downsides-hope
Leon F Seltzer Ph.D.
Posted July 25, 2018 Reviewed by Ekua Hagan

Throughout history, hope has been viewed favorably, as virtually essential to our welfare. True, many writers have inveighed against “false hope.” But it’s generally been perceived as a positive, almost essential, motivating force. And in any case, it seems inextricably woven into the fabric of human nature.
Take the famous line from 18th century English poet Alexander Pope: “Hope springs eternal in the human breast.” And far more recently, writing for Blogspot (10/24/11 ), a physician in training named Isaac suggests pretty much the same thing—though here the tone is unquestionably cynical toward this abiding universal tendency:
I hate the word ‘hope.’ It’s a cruel and bitter emotion that won’t leave you alone. In meditation, one is taught to ‘let go’ of attachments to emotions. I can often do that with anger and grief and anxiety … but not hope. I despise it because even if I let go, it never lets go of me.
Other writers as well have investigated the “darker side” of hope, elaborating on how it can actually ensnare you, and far more than you might think. So it’s of considerable practical value to explore the often unrecognized problems with such a curiously optimistic—or aspirational—emotion.
In reviewing the literature on this most paradoxical of subjects, I’ve come up with no fewer than seven “downsides” related to hope. All of them merit scrutiny since it’s crucial to distinguish between good hope and bad.
Put simply, not all hope deserves to be regarded as advantageous; an asset. And because its positive facets are much more publicized than its adverse ones, this post will focus on why it’s a good idea to be mindful of how certain kinds of hope—as well as degrees of hope—can wind up defeating you. For, as the acclaimed German philosopher Nietzsche (admittedly) overstated the case: “Hope in reality is the worst of all evils because it prolongs the torments of man.”
So, let’s examine the many negatives that have been linked to hope, so we can better grasp the at least partial truth of Nietzsche’s extraordinary pessimism about this expectational feeling.
1. Hope can be an inherently biased ideal.
Overall, it’s better to have a positive, or optimistic, bias than a stubbornly negative one. But ideally, when we make an evaluation, or come to a conclusion, we ought to base our judgment on logic and rationality—rather than on hope, desire, extravagant fantasies, or a relentless longing for change.
If we lived in a utopia, and so were justified in believing that whatever we wanted would inevitably materialize, then we wouldn’t need hope at all. But given the actual world we inhabit, we’re better off avoiding as much biased hope as possible.
Finally, if we want to succeed and feel fulfilled in life, we need to temper the idealism that “grants” us hope with the hard, unalterable facts of reality.
2. Hope can set us up for disappointment and defeat.
The emotion of hope pertains to that which hasn’t yet transpired. So it’s only natural that the more favorable our expectations of the future, the greater will be our disappointment—or disillusionment—when these expectations aren’t met or are irrevocably crushed.
In this sense, it’s much better to consciously restrain our hopes so we can also limit the hurt that a defeat, failure, or setback likely would engender. Hoping may be pleasurable, but hope defeated can be quite painful.
Consequently, it’s useful to keep in mind that anticipating favorable results is not without its hazards and that these risks are best reflected upon in advance.
3. Hope can hamper us from adequately preparing for negative outcomes.
A flexible, forward-looking mindset is almost always preferable to a rigidly fixed one. But there are many situations in which a realistic acceptance of a possibly (or likely) negative outcome is more beneficial than clinging to a hope counter to what is quite probably (if not certainly) going to happen. If the odds of a favorable outcome are little to none, it just makes sense to moderate our perspective so that it’s more in line with real-life eventualities.
If you’re definitively diagnosed with terminal cancer, for example, and resolve to begin making peace with your mortality, accepting the fate that sooner or later awaits you, you’ll thereby optimize the chance of experiencing “a good death.” You’ll say your fond farewells to loved ones, express feelings that till now you’ve kept buried, and tie up whatever loose ends in your existence you can, completing your days in a state of gratitude for everything life offered you—even as you reconcile yourself to what it didn’t. Realistically, the only way to “triumph” over death is to embrace it as an intrinsic, though terminal, aspect of life.
Compare this openness and receptivity in coming to terms with your ultimate demise to the obdurate determination to fight your fate till the bitter end, as though resisting what’s inescapable will assist you in bravely contesting your mortality. That’s simply denying your part in the human condition. And that’s not just grandiose, it’s also foolhardy.
Yet rather than cultivating humility and fortitude in the face of imminent death, many people willfully choose to turn their back on what’s best encountered head-on. To be sure, mounting a monumental fight against one’s ineluctable fate is frequently viewed as courageous. But a much stronger argument could be made that it takes more courage to open-heartedly accept it.
Consider what various writers and researchers have had to say about this reality-refuting aspect of hope:
Michael Schreiner, in his “The Problem With Hope” (11/13/15) , notes that “it’s easy to confuse the idea of mindful acceptance with unhealthy states of being like giving up, complacency, or settling for less.”
And Cathal Kelly, in her “Study Finds a Downside to Hope” (11/06/09) , reports on a University of Michigan research team that “followed patients who had their colon removed. One group knew the procedure was permanent [while] the second group was told that after a period of healing, their bowels could be reattached. / After a few weeks, both groups were struggling. But six months later, the group that had been permanently disabled showed far more life satisfaction. . . . The group awaiting a reversal procedure remained depressed and unhappy. / “They knew things would get better [concluded the team’s leading investigator] but that made them less satisfied with present circumstances. . . . While usually a good thing, we see that hope has a dark side.”
In this same article, the author goes on to quote Dr. David Casarett, a hospice physician and senior fellow at the University of Pennsylvania’s Center for Bioethics: “Our job as physicians is to point people toward the sort of hope that is achievable.”
And later in this piece, Kelly quotes yet another physician on the matter—the late British physician Robert Buckman: “Even if the news is bad, even in some respects hopeless, it allows you to know what you’re dealing with, and you can cope” [vs., that is, hope].
4. Hope can be like prayer: wishing for something rather than more forcefully working toward it.
Not always, but definitely sometimes, hope inhibits taking necessary, or advisable, action. That is, hoping or praying for something doesn’t in itself imply doing anything about it. Rather, it can keep you in a holding pattern rather than prompting you to act to “achieve” your hopes.
One author suggests that, even more than this, it can be understood as a kind of “moral cowardice” (from Simon Critchley’s “Abandon (Nearly) All Hope,” New York Times, 04/19/14) . And whether this sort of hope comes from an enduring belief in a beneficent God or from a more secular position, all too often it leads to passivity—as though if you only wish hard enough for a desired outcome such an affirmative stance alone will maximize its possibility.
But here again, consider the research. An article entitled “The Problem With…Hope” (farnishk, The Earth Blog, 01/24/08) , in which the author refers to “a widely cited and carefully controlled study into the relative effects of prayer on post-operative coronary recovery” (see AHJ: American Heart Journal, 2006, 151, 934-942) “found no significant difference in recovery rates between those who received prayer unknowingly and those who did not receive prayer at all”—and also that “the group of patients who knowingly received prayer had a 15-20 percent worse recovery rate than the other two groups.
5. Hope can encourage you to forfeit personal power and control.
Closely related to the above, passively hoping for a desired outcome can be tantamount to relinquishing any responsibility for making it happen. Resignedly, you could be giving yourself the message that you can’t do anything about the situation when, quite possibly, you actually could. Once you give something over to an external force, then, practically, you’re “surrendering” to it.
So far as I could determine, this hypothesis has yet to be researched, but it’s reasonable to assume that the motivation to give one’s all to an upcoming challenge would be diminished by that person’s looking for some deus ex machina to almost magically intervene on their behalf. Too often, hope is susceptible to drift—or degenerate—into mere wishful thinking.
The Earth Blog author cited in #4 succinctly characterizes such hope as a “dereliction of responsibility.” And he notes that this breach in the populace’s handing over to various authorities what, finally, they must each take responsibility for refers not only to religious leaders but also to politicians, heads of corporations, and even environmental organizations. Such a regrettable phenomenon represents for him nothing less than “a mass [my emphasis] dereliction of responsibility.”
And the author closes his critical piece with this wonderfully suggestive quote: “When hope dies, action begins” (from Derrick Jensen, Endgame ).

6. Hope can be a tool of self-deception.
False hope is a hope that has no meaningful basis in reality. It’s self-deluding, and eventually it will probably end up sabotaging or defeating you. So you need to ask yourself whether what you’re hoping for makes any legitimate sense, or whether it simply makes you more gullible. For when hope literally runs away with you, your ability to see things clearly—and with just the right degree of skepticism—is seriously undermined.
Consider, for instance, hoping that you’ll win the lottery (after all, someone’s got to win!) or, more generally, standing up to forces far more powerful than you and with the law on their side. Such excessively aspirational hope isn’t only irrational, it’s also imprudent and can at times be dangerous. For it can increase the risk that you’ll get into more trouble than you might already be in. What is it but hope that creates our most wondrous, but farfetched, fantasies. But, enjoyable as they may be, to the extent that they’re over-the-top, it’s wise to maintain them as fantasies only.
7. Hope can set us up for hopelessness.
When hope is defeated, and possibly repeatedly defeated, it’s vulnerable to be replaced by hopelessness—or downright despair (which means the complete absence of hope). And once hope weakens or vanishes, it’s all the harder to take action that could be effective in helping you reach your goals.
On the contrary, if you proceed in your endeavors without hope, independently striving to accomplish whatever objectives you’ve set for yourself, you’ll be taking full responsibility for your future. And regardless of whether you succeed or fail, you’ll be able to attest to—and maybe even congratulate yourself for—all the industry, zeal, and perseverance you put into your attempts. That’s finally far more affirmative than “helplessly” depending on providence to enable you to overcome personal obstacles. Though putting your trust in hope can be extremely tempting, diligently applying yourself to what you most care about is a much more reliable way to prosper in life.
Speaking of the Greek philosophy of Stoicism, Darrell Arnold, Ph.D., discusses how Stoics saw inner peace as linked to eliminating hope, because hopes are eventually dashed. Moreover, the Stoics saw the emotion of anger as originating from
misplaced hopes smash[ing] into unforeseen reality. We get mad, not at every bad thing, but at bad, unexpected things. So we should expect bad things . . . and then we won’t be angry when things go wrong. Wisdom is reaching a state where no expected or unexpected tragedy disturbs our inner peace, so again we do best without hope” (from “Is Hope Bad?” Reason and Meaning, 3/14/17).
Better, that is, to accept the world as unfair and then focus on what, nonetheless, might be possible for you to change.
To conclude, it’s not bad to hope—if, that is, you hope wisely. Still, if you earnestly dedicate yourself to what you want to happen, not really trusting in hope but (self-confidently) in your own tactical and prudent efforts, then hope may become redundant—and even be an impediment. As already indicated, when your hopes are false or unrealistic, you can end up feeling not simply frustrated and disappointed but also angry and resentful . . . and possibly embittered as well.
So, if you wish, go ahead and hope. But do so judiciously.
© 2018 Leon F. Seltzer, Ph.D. All Rights Reserved.
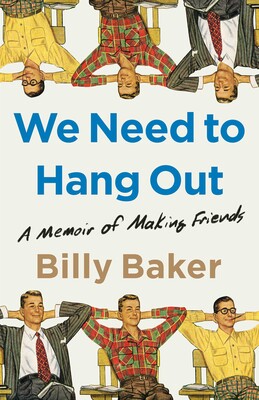
We Need to Hang Out: A Memoir of Making Friends
Addressing the Male Depression and Loneliness crisis that is ongoing.
Rory
https://www.simonandschuster.com/books/We-Need-to-Hang-Out/Billy-Baker/9781982111083
In this comic adventure through the loneliness epidemic, a middle-aged everyman looks around one day and realizes that he seems to have misplaced his friends, inspiring him to set out on a hilarious and ultimately moving quest to revive old tribes and build new ones, in his own ridiculous way.
At the age of forty, having settled into his busy career and active family life, Billy Baker discovers that he’s lost something crucial along the way: his friends. Other priorities always seemed to come first, until all his close friendships had lapsed into distant memories. When he takes an assignment to write an article about the modern loneliness epidemic, he realizes just how common it is to be a middle-aged loner: almost fifty million Americans over the age of forty-five, especially men, suffer from chronic loneliness, which the surgeon general has declared one of the nation’s “greatest pathologies,” worse than smoking, obesity, or heart disease in increasing a person’s risk for premature death. Determined to defy these odds, Baker vows to salvage his lost friendships and blaze a path for men (and women) everywhere to improve their relationships old and new.
In We Need to Hang Out, Baker embarks on an entertaining and relatable quest to reprioritize his ties with his buddies and forge more connections, all while balancing work, marriage, and kids. From leading a buried treasure hunt with his old college crew to organizing an impromptu “ditch day” for dozens of his former high school classmates to essentially starting a frat house for middle-aged guys in his neighborhood, he experiments with ways to keep in touch with his friends no matter how hectic their lives are—with surprising and deeply satisfying results.
Along the way, Baker talks to experts in sociology and psychology to investigate how such naturally social creatures as humans could become so profoundly isolated today. And he turns to real-life experts in lasting friendship, bravely joining a cruise packed entirely with crowds of female BFFs and learning the secrets of male bonding from a group of older dudes who faithfully meet up on the same night every week. Bursting with humor, candor, and charm, We Need to Hang Out is a celebration of companionship and a call to action in this age of alone.
Job Burnout: How to spot it and take action
https://www.mayoclinic.org/healthy-lifestyle/adult-health/in-depth/burnout/art-20046642
Feeling burned out at work? Find out what you can do when your job affects your health.
Job burnout is a special type of work-related stress — a state of physical or emotional exhaustion that also involves a sense of reduced accomplishment and loss of personal identity.
“Burnout” isn’t a medical diagnosis. Some experts think that other conditions, such as depression, are behind burnout. Some research suggests that many people who experience symptoms of job burnout don’t believe their jobs are the main cause. Whatever the cause, job burnout can affect your physical and mental health. Consider how to know if you’ve got job burnout and what you can do about it.
Job burnout symptoms
Ask yourself:
- Have you become cynical or critical at work?
- Do you drag yourself to work and have trouble getting started?
- Have you become irritable or impatient with co-workers, customers or clients?
- Do you lack the energy to be consistently productive?
- Do you find it hard to concentrate?
- Do you lack satisfaction from your achievements?
- Do you feel disillusioned about your job?
- Are you using food, drugs or alcohol to feel better or to simply not feel?
- Have your sleep habits changed?
- Are you troubled by unexplained headaches, stomach or bowel problems, or other physical complaints?
If you answered yes to any of these questions, you might be experiencing job burnout. Consider talking to a doctor or a mental health provider because these symptoms can also be related to health conditions, such as depression.
Possible causes of job burnout
Job burnout can result from various factors, including:
- Lack of control. An inability to influence decisions that affect your job — such as your schedule, assignments or workload — could lead to job burnout. So could a lack of the resources you need to do your work.
- Unclear job expectations. If you’re unclear about the degree of authority you have or what your supervisor or others expect from you, you’re not likely to feel comfortable at work.
- Dysfunctional workplace dynamics. Perhaps you work with an office bully, or you feel undermined by colleagues or your boss micromanages your work. This can contribute to job stress.
- Extremes of activity. When a job is monotonous or chaotic, you need constant energy to remain focused — which can lead to fatigue and job burnout.
- Lack of social support. If you feel isolated at work and in your personal life, you might feel more stressed.
- Work-life imbalance. If your work takes up so much of your time and effort that you don’t have the energy to spend time with your family and friends, you might burn out quickly.
Job burnout risk factors
You might be more likely to experience job burnout if:
- You identify so strongly with work that you lack balance between your work life and your personal life
- You have a high workload, including overtime work
- You try to be everything to everyone
- You work in a helping profession, such as health care
- You feel you have little or no control over your work
- Your job is monotonous
Consequences of job burnout
Ignored or unaddressed job burnout can have significant consequences, including:
- Excessive stress
- Fatigue
- Insomnia
- Sadness, anger or irritability
- Alcohol or substance misuse
- Heart disease
- High blood pressure
- Type 2 diabetes
- Vulnerability to illnesses
Handling job burnout
Try to take action. To get started:
- Evaluate your options. Discuss specific concerns with your supervisor. Maybe you can work together to change expectations or reach compromises or solutions. Try to set goals for what must get done and what can wait.
- Seek support. Whether you reach out to co-workers, friends or loved ones, support and collaboration might help you cope. If you have access to an employee assistance program, take advantage of relevant services.
- Try a relaxing activity. Explore programs that can help with stress such as yoga, meditation or tai chi.
- Get some exercise. Regular physical activity can help you to better deal with stress. It can also take your mind off work.
- Get some sleep. Sleep restores well-being and helps protect your health.
- Mindfulness. Mindfulness is the act of focusing on your breath flow and being intensely aware of what you’re sensing and feeling at every moment, without interpretation or judgment. In a job setting, this practice involves facing situations with openness and patience, and without judgment.
Keep an open mind as you consider the options. Try not to let a demanding or unrewarding job undermine your health.
‘We Need To Hang Out’
Studies have shown men have trouble maintaining close friendships, and that has detrimental effects. NPR’s Rachel Martin talks to Boston Globe reporter Billy Baker about his book: We Need to Hang Out.
How many friends do you have? I’m talking about really good friends. Now think about how long it’s been since you spent time with them. When Boston Globe reporter Billy Baker’s editor assigned him to write a story about friends back in 2017, he discovered that he had lost touch with nearly all of his. And like many men around his age – he was about 40 at the time – he found himself pretty lonely. Researchers told him that even before the pandemic hit, Americans were becoming increasingly isolated from their friends. And men are doing way worse than women. So in his new book, Billy Baker writes about his attempts to reconnect with his friends. The book is called “We Need To Hang Out.”
BILLY BAKER: I’d be perfectly happy if nobody gets more than five pages into this book and they’re like, I know what I need to do. I need to hang out with my friends.
MARTIN: And if you do keep reading, you’ll realize it can be more complicated than that – and more dire. Responsible for many ailments, both mental and physical, loneliness is killing us.
BAKER: Isolation, even living alone – all these, like, little things, can make you more susceptible to basically everything you don’t want. When I wrote this article, people wrote to me – and emails came by the thousands, these really confessional emails. They weren’t so much interested in the information about the cancer. They wanted to know about the cure. I wanted to know about the cure for myself, you know? I wanted to know how to be friends with my friends in this period in life – you know, this broad period we call middle age – where there’s so many other things begging for your attention that friends, you know, wasn’t one of the priorities when I woke up every morning.
MARTIN: Your friend Rory, for example, had up and moved to Vienna, Austria, and never told you about (laughter).
BAKER: Never mentioned it. I write this article. I send it to him. I’d mentioned him in the article. And it was like, oh, this – you’re not going to be happy to hear this. But I forgot to tell you, I moved to Vienna. And this was a guy I would have considered my best friend in the world. And so – you know, I did a lot of things on this journey. And the first thing I did was chase him to Vienna. It felt very…
MARTIN: This is so dramatic, Billy, though. Like, you could have started with a FaceTime call.
BAKER: I mean, I guess. But I was just still in shock at the whole thing. And – plus, you know, I’ve never been to Vienna. So you know, like, I hop on a plane. It felt very, like, romantic comedy scene as I’m, like, dashing to the airport and like, what am I doing? I’m getting on this plane to save a relationship with a guy. Like, this is new territory for me. But you know what? Like, that was the beginning of a pattern that held throughout this entire journey, where just showing intent and showing a teeny little bit of vulnerability, like not a cool-guy move, it always led to the best places. And he will never move to another country without telling me again.
(LAUGHTER)
MARTIN: Can we talk a little bit about that cool-guy thing and what’s embedded in that? While you don’t use these words in the book, you do seem to suggest that some of that bias against intimacy is a bias against behaviors that are seen as feminine. Is that fair to say?
BAKER: I think it is fair to say. One of the things that I kept hearing right from the beginning of this is how women are so much better than men, and all the data seem to support it. Women are better at friendship than men. And it was like, OK. Like, why? Like, what is it that they do? And women are more willing to touch. They’re more willing to call each other when they’re feeling down. They’re able to keep up relationships over the phone in ways that men are not.
So it’s actually a very interesting, fundamental difference in the way men interact versus the way women interact. Men talk shoulder-to-shoulder, and women talk face-to-face. So immediately, like, male friendships are built – usually built around activity. You know, we’re doing something together. Like, a friend of mine referred to golf as his way of finding something to do with his hands while he talks to his friend about, you know, what’s going on at home.
MARTIN: Through the book, it’s you setting this intention to cultivate friendships – trying to nurture old ones, also start new ones. You start sort of an unofficial fraternity with a wider group of guys. Some of them you know really well, some you don’t. Can you talk about that moment when you’ve invited this group – what is it, 12 guys? – very intentional number…
BAKER: Yes.
MARTIN: …To this place, this barn you’ve secured to begin this regular hangout thing. How did you explain what you were doing there when you got up in the barn and said, welcome…
BAKER: (Laughter).
MARTIN: …Dudes?
BAKER: Well, I mean, the idea was, all right, I’m going to try and build a new tribe. I’m going to try and connect these guys that I’ve met. You know, maybe they’re through my kids, maybe wherever and I felt a little bit of a spark. Like, OK, we could be friends. So I brought them all together. Maybe it didn’t have to be this dramatic, but I invited them all. I sent them all sort of invitations, didn’t tell them what was up. I kind of laid out this whole journey I was on. The energy in that room was that like, yeah, we could also use someone to hang out with on a Wednesday night. It wasn’t a slight on our friendships of the past to say we need a better daily friend life in the present.
MARTIN: But you do ponder whether just the hangout is sufficient. You go through this part of the book where you think you need a purpose, a task – that it’s not enough to just sit around and, you know, shoot the bull, so to speak. You have to be physically doing something – shoulder-to-shoulder, right?
BAKER: Yeah. For a while, this Wednesday night crew was going gangbusters. And then it just – it was like, what are – we’re just going to get together in this barn and do what – like, talk about our feelings? I use this phrase in the book, velvet hooks. There are these things that connect people. And they’re soft. You’re not locked in iron – the weekly golf game, the fantasy football, the bar trivia, the book clubs, the sports teams, whatever it is, you know. They’re the excuse to get together. And then, you know, while that activity is going on, maybe that’s where the magic happens.
And it’s funny. What really brought everyone together – a guy came up with the idea, let’s build, like, a dirt BMX track like every little kid’s dream. By simply agreeing that that’s what we were going to do, it gave the group a purpose. And we haven’t done it. But we do get together…
MARTIN: (Laughter).
BAKER: We do talk about how we’re going to do it. And then, you know, we…
MARTIN: That’s so interesting, though. The dream is enough. The dream is the velvet hook.
BAKER: But it works. It works for us. And at this point, we have become good enough friends where the awkwardness is gone. And I love it. I live for it.
MARTIN: Billy Baker – his new memoir is called “We Need To Hang Out.” Billy, thanks so much for talking with us.
BAKER: Thank you, Rachel. I enjoyed it.
(SOUNDBITE OF SONG, “WHY CAN’T WE BE FRIENDS”)
WAR: (Singing) Ooh, ooh, ooh…