Category: EMDR / TRAUMA
Emotional Flashbacks: What They Feel Like, And How To Cope With Them
Privacy Overview
EMDR in a Nutshell: Healing from Trauma
What Is EMDR?
Eye Movement Desensitization and Reprocessing (EMDR) is a guided process that supports trauma work by using “bilateral stimulation” (BLS), or stimulating each hemisphere of the brain alternately via the senses. EMDR also involves talking, deep breathing, and other ways of grounding the nervous system. (“To ground” the nervous system means to bring its level of activation back or closer to the “ground” or baseline level.)
There are many kinds of BLS that can work well, although eye movements have been shown to be the most effective. In my practice, I use a combination of eye movements (watching a light or my finger moving back and forth), as well as sounds alternating in each ear through headphones—whichever the client prefers.
When we first meet, I work together with my client to figure out what combination of sounds and colors feels best. (A person’s own report is the best indicator for what kind of stimulation works best for them.)
Rather than medicalizing distress, EMDR provides a way of healing from trauma. EMDR isn’t about trying to treat the symptoms of an illness. It’s about healing from the root cause.
What Can EMDR Treat, and What Is It Not Helpful for?
EMDR can be very useful for trauma, specific anxieties and phobias, and many forms of impact left behind by difficult experiences or relational patterns. EMDR can be effective for Complex Post Traumatic Stress Disorder (C-PTSD) and developmental traumas.
Another form of EMDR called Eye Movement Desensitization (EMD) can be helpful to reduce distress due to overwhelming or complex traumas and triggers, which can be used in place of or in preparation for additional reprocessing.
EMDR can be used to prepare for specific future actions (public speaking being one common example).
It is even possible to use EMDR for memories that may be vague, pre-verbal, or otherwise not fully available to consciousness. This is accomplished by processing the physical responses and triggers we have in the present.
EMDR is less directly useful for depression, grief, the impact of neglect, and other experiences we might characterize with the word “lack.” Many or most forms of difficult human experience involve both fear and loss, and working on the somatic or body-based reactivity to trauma with EMDR can allow grief work to become tolerable. In other words, EMDR can open the way for other therapies (such as psychodynamic, existential, and other “talk” therapies) to be more effective.
What Is the Difference Between a Traumatic Memory and Other Memories?
Each memory we have is stored in a “neural tree,” which (in theory) is a structure of cells that we could pick up and look at. Our non-traumatic or ordinary memories have many “branches” into the frontal cortex of the brain, which allows us to describe the memory with language, and into the hippocampus, which allows us to put the experience into the context of time (i.e. we know it happened in the past and therefore that it is now over).
Conversely, the neural trees of traumatic memories have fewer of these branches, and they also have a greater number of “roots” that anchor them to the amygdala, which is the fight/flight/freeze center of the brain. (“Freezing”, or dissociation, can be thought of as a protective numbing response to the “fight or flight” responses of anger, anxiety and fear. “Drifty,” “numb,” and “confused” are some words clients who experience dissociation have used to describe how it feels to them.)
This makes it much easier for a traumatic memory to activate the adrenal glands, and thereby the threat response system throughout the whole body. This is what we mean when we colloquially use the word “trigger”: the body has been activated for survival in response to a present stimulus that is meaningfully reminiscent of the past.
What Is Trauma Work?
“Trauma work,” “trauma processing,” or just “processing” are all shorthand ways we refer to helping neural trees grow more branches and untwine their roots! EMDR can make this process much easier and faster, though the process itself is ancient. We say that the brain “knows” how to heal itself, much like how the skin “knows” how to heal a cut. EMDR gives the brain support—much like how antiseptics and bandages can support healing wounds of the skin.
As we said above, unprocessed traumatic memories are less connected to the frontal cortex. This means we have less ability to use language to “look at” the memory, instead of “be in it,” and it’s much harder for our systems to believe that the memory is in the past and that the threat is over—it can feel like it’s happening all over again. “Naming it to tame it,” or putting experience into words (which, in EMDR, happens between doses or “sets” of BLS), helps grow more connections to the frontal cortex.
Another reason doing trauma work is one of the greatest challenges we face is because the brain and body don’t have a system that tells us we are in “mild distress.” We can only adjust between “life and death (fight, flight or freeze)” and “calm (rest and digest).” Recalling traumatic memories, alternating with taking breaks, helps the “roots” into the amygdala unwind and the survival system to quiet.
So even contemplating trauma work can feel like life and death! It’s important to be aware that there’s a reason for this intensity, and that after successful processing, it will fade. Working on trauma is not likely to be comfortable, but if it is not tolerable for my client, we stop (using a stop signal we agree on before we begin). If that happens, we focus on support and using grounding skills until their nervous system is closer to baseline. Trauma work is not as hard as trauma!
How Does EMDR Work?
EMDR allows us to process trauma by activating traumatic memories at the same time as it gives the nervous system cues for safety. This creates an “in and out” rhythm, which helps the brain get back in sync, and supports your brain in building connections to the neurons that store these memories.
We have data that clearly show that EMDR gets good results. Science is still exploring the reasons why EMDR works, but here are some of the most popular current theories, one or all of which could be true:
- The back-and-forth visual motion communicates to the amygdala that your body is in motion, which tells the brain that it is safe, active, and not trapped.
- The ocular nerve or other sense organs are stimulated, the activity of which facilitates rewriting (basically, it gets the area “warmed up” and ready for change).
- Stimulation of the sense organs takes up some of the brain’s bandwidth and resources (such as oxygen and glucose), which means less is available to fuel panic responses.
- The eye moments mimic what happens in REM sleep, another time when the brain is processing and storing memories. (This process is not fully understood, but it’s theorized to be similar to how EMDR and BLS work.)
- Trauma disrupts the natural rhythm of brainwaves, and EMDR provides a “corrective” rhythm to resonate with the brain as it processes disruptive memories.
- Predictable structure while talking about trauma is distracting and calming.
Any form of verbalizing trauma while in the regulating presence of a trusted other will have beneficial effects, for at least two reasons. First, “If you can name it, you can tame it”: Language activates the frontal cortex, which helps to build neural bridges, as well as causing a release of endorphins and other soothing neurotransmitters.
Second, our nervous systems are built from birth to monitor the internal state of others (including breath and pulse rates), and to resonate with them—so sharing a story with someone who is calm can help us calm ourselves while we tell it.
What Happens During an EMDR Session?
EMDR has a few different phases. In the first phase, I lay the groundwork with my client, including practicing grounding skills, setting up a stop signal, getting more familiar with BLS, and making sure they have a crisis plan and other supports in place in case they need help between sessions.
Next, we work together to come up with some “headlines” of memories to target, and explore the client’s feelings and beliefs about these memories. This doesn’t mean it’s not ok if we discover more along the way, but it can help us find some good places to start. In fact, we might say that it’s more likely than not that other memories will come up. That’s neither good nor bad, it’s just the brain going through the networks of association it has.
If relevant, we may also set goals at this point for a future action the person is working towards.
Most often, BLS is not used until session two (although this does not mean that processing cannot begin in your brain before that!). At that point, I work with the person to bring up the memory we agreed to use as a starting point, paying attention to the sense information, body feelings, and emotions that go with the memory.
Then, we do about 20 to 30 seconds of BLS. During that time, I ask my clients to “just notice,” “go with,” or “follow” what they’re noticing inside themselves. At the end of every “set,” I ask them to take a deep breath, tell me a sentence or two about what they’re noticing, and then we repeat.
It’s kind of like you’re on a train ride, and I’m on the phone with you, asking you what you see out the window.
Sometimes, what a person feels and notices from set to set will change, and sometimes it won’t. It’s even perfectly normal to have periods of feeling nothing at all. This is often the brain’s way of resting, assessing safety and connection, or otherwise taking care of you, and sometimes the best thing to do is just notice that feeling for a few minutes.
Although I keep a close eye on how my client is feeling as we go, I trust their own report most of all—as a person is their own best guide to how they’re doing. Some experiences are not always visible from the outside, such as “red lining” (panic, fury, etc.) or “blue lining” (dissociating).
I always tell my clients that if they think they’re feeling too much or too little, or are otherwise outside of their “zone of tolerance,” it’s important for the healing of their nervous system that they let me know. That way, we can take a break and use grounding skills before we continue.
Most sessions are spent doing sets for about 20 to 40 minutes. At the end of every session, we wrap up by using grounding skills to return the person’s nervous system to a tolerable state. I also ask if there’s anything they want to “leave in the container of therapy” (which doesn’t mean it won’t come to mind between sessions, but rather that they will set the intention not to continue to focus on it). Then we check in for a minute or two so we can both share thoughts and observations about the session.
Reprocessing can take several sessions. On average, it ranges from 3 to 12 weeks, though it can be significantly shorter or longer. Sometimes a person may feel different by the end of a session, and sometimes they may not.
What Do I Do Between Sessions?
In between sessions, clients may continue to process memories, meaning they may still be remembering, feeling, or even dreaming things. If that happens, their job is to notice it as much or as little as they’d like to, and then use a grounding skill. (“They don’t work if you don’t use them!”)
The client’s most important job, and their only “homework,” is to keep their nervous system and emotions within tolerable limits as much as they can. (It’s ok if they can’t do this perfectly, but it’s important to set it as a goal to strive towards.)
There are a number of questions we check in about as we prepare to engage in EMDR:
- How will you know if you’re outside of your tolerable zone?
- What grounding skills will you use?
- What friends and family can you connect with, whether to ask for help using grounding skills, talk about what you’re feeling, or just to share space?
- If you are unable to ground yourself on your own or with the assistance of loved ones, what hotlines and/or mental health professionals will you call and how?
What Might Be Different After EMDR Is Complete?
The good and bad news is that EMDR does not make you forget what has happened. After processing, accessing memories of a traumatizing event will feel much like accessing any other memory. The most noticeable difference will likely be that the memory no longer creates an overwhelming body response.
After EMDR, it’s common for a phase of grief work to begin. This can involve feeling sadness and anger, as well as (in some cases) shifts in sense of identity or what is important to us. Sometimes we need support to explore questions like “Who am I without this fear?” or “Is it ok to get better?” Continuing in talk therapy after EMDR is over may help people continue to integrate their experiences and to heal.
To anyone contemplating EMDR, I wish you good healing, and congratulations to anyone who is willing to take the risks to talk about the hard stuff. I believe the greatest gift we can give to ourselves and to others is to make room for our feelings.
Fawn Response: A Trauma Response + The Reason for People-Pleasing Behavior | Modern Intimacy
Source: Fawn Response: A Trauma Response + The Reason for People-Pleasing Behavior | Modern Intimacy

When the going gets tough in your relationships, what is your gut reaction? Do you feel like you spend most of your time pleasing other people? Or do you have a hard time knowing how to meet your needs? Maybe you feel like you don’t see a fight response or flight response in yourself, but you notice one of the two lesser-known responses: the freeze and fawn responses.
You might be wondering, what exactly are the freeze and fawn responses? Two of the four trauma responses (fight, flight, freeze, and fawn) that can stem from childhood trauma, and they both involve symptoms of PTSD (Post-Traumatic Stress Disorder). A fawn response occurs when a person’s brain acts as if they unconsciously perceive a threat, and compels survival behavior that keeps them under the radar.
What is the Freeze Response?
This response is paralyzing. You are so overwhelmed by fear that your body stops.
You stop thinking, stop moving, and, in some cases, stop breathing.
Because your body stops, it is an unconscious act of dissociation with whatever is happening around you. This response is also associated with “shell shock” or basic post-traumatic reactions. If you have the “freeze” response early in life, you may be predisposed to experience freeze symptoms later in life.
What is the Fawn Response?
Different from the fight, flight and freeze responses, the fawn response points to people-pleasing.
Though people-pleasing is not the only manifestation of fawning, it tends to be the most evident sign.
Pete Walker was a pioneer in defining “fawning.” Walker says this response is developed in childhood to avoid mistreatment from adults.
Fawn responses can be any number of things but are nervous attempts to deflect attention. This can mean flattery, admission to toxic relationships, or complete destruction of personal boundaries.
People who fawn tend to deny their preferences and boundaries to make other people happy. They unconsciously believe that the price for relational security is compliance. They think that if they make others happy, they will be in less danger.
Do I Show the Fawn Response?
Sometimes those who show the fawn response don’t even know they are fawning, and they have likely experienced positive feedback from others in return, so it may not register as a problematic behavior.
Think you may fall into this category? Think back to any time conflict has come up. You can start by asking yourself these questions to find out:
Do I put my needs aside to make others feel better?
Do I feel empty in relationships after giving too much of myself?
Do I avoid conflict at all costs?
Do I feel everyone’s emotions all at once?
Do I think I am responsible for making everyone happy?
If you answered yes to more than two of these questions, it is likely your default is the fawn response.
Why Do I Have a Fawn Response?
There is not a short answer to why someone may show the fawn response. Generally, those that fawn are extremely empathetic and would rather take the emotional blow than someone else, the price of admission in relationships, and fawn types seek safety in interpersonal dynamics.
The most popular theory on fawning comes from Adverse Childhood Experiences (ACEs.) These are events usually happen before the child is eighteen years old and can impair children for the rest of their lives.
Adverse Childhood Experiences can range from poverty to neglect to abuse at home. Continuances of these events can establish negative thought patterns early-on.
When our brains are still developing, we will do anything to avoid danger. The fawn response is to seek safety by merging with the perpetrator. So as children, we do what we are told, even if it isn’t what is right or good for us.
This response invokes strategies from “flight,” “flight,” and the “freeze” responses, so it is seen as the most adaptive reaction. Fawning requires knowledge of whomever is hurting you and skill to know how to appease them. It is often seen in people who endure narcissistic abuse.
Fawning is also sometimes associated with codependency. Both are emotional responses that are triggered by complex PTSD.
In both fawning and codependency, your brain thinks you will be left alone and helpless. The brain’s response is to then attach yourself to a person so they think they need you. This can lead to do things to make them happy to cause less of a threat to yourself.
Though, the threat is the variable in each scenario. In fawning, the threat could be social isolation, conflict with a loved one, or unhappiness. Codependency is generally paired with loneliness.
How Can I Help My Fawn Response?
Trauma affects everyone, not just the one experiencing the trauma.
It affects the one inflicting the trauma, the one affected by the event, and anyone who interacts with those people.
The fawn response is a great example of this since it involves submitting to what others want.
So, how can you begin healing from trauma?
Observe Yourself
One of the first things to do to stop fawning behaviors is to observe them.
Whenever you are triggered, think about these things:
Why am I fawning right now?
How am I experiencing fawning behaviors?
How do I feel right now?
What do I want to do right now, not how do I think I need to react?
Asking yourself these questions will begin to unlock the trauma-affected regions of your brain.
Therapy
A next possible step is to enroll in therapy appointments. Being able to share your trauma with a professional can help you process. Not only will you have a listener, but someone who can offer science-backed suggestions!
There are several different methods for healing trauma, including the Eye Movement Desensitization and Reprocessing (EMDR) process. This system helps re-wire your brain, creating new neurological pathways that help you react to trauma when it comes up.
Taking stock of your fawning behaviors before going to therapy is good. You can fill your therapist in on the issues since they likely will not see your trauma responses themselves.
Many times, you learn about traumas you weren’t didn’t even know were affecting you.
Find a Safe Person
Aside from a therapist, find a person you can talk with about your recovery. This can be a friend or family member that can hold you accountable.
As you’re healing, they will ensure you continue taking steps to stop fawning behaviors. But, they will also be the first ones you call when you’re struggling!
Next Steps
If you are ready to face your fawn response, to improve your mental health, there are many steps you can take. Begin thinking on ways to stop your fawning behaviors and how to ask for help from trusted people. There is no need to be obsessive compulsive about it, though. The main thing to remember is that other people have benefited from your fawn response, so they may have reactions to your changes.
Don’t worry, you can open up little by little and practicing the art of saying no more readily. Grab a cute mug that promotes positivity and healing. Write something that describes how you’ve been feeling. Or, try a yoga class to deepen your mind-body connection.

Author Bio
FREE 30 MIN INITIAL CONSULTATION WITH
MODERN INTIMACY …
You May Also Like…
The Reality of Military Sexual Trauma & What To Do
Members of the armed forces experience stress that ordinary civilians do not. Imagine being a part…
The Orgasm Gap: Solutions for Boosting Sexual Pleasure
Everyone deserves an exhilarating sex life. While orgasms aren’t the only source of pleasure…
10 Internalized Misogyny Books That Can Set You Free From the Patriarchy
Did you know that feminism is the belief that both sexes should have equal opportunity in all…
0 Comments
Submit a Comment
LET’S WORK TOGETHER
WANT TO WRITE FOR MODERN INTIMACY?
What are the signs and symptoms of dissociation and dissociative disorder?
Source: What are the signs and symptoms of dissociation and dissociative disorder?
Dissociation and dissociative identity disorder (DID)
This section gives information about dissociation and dissociative disorders. It explains the different dissociative disorders, their symptoms and treatments. This section is for anyone with dissociation and dissociative disorder and their carers, friends or relatives.
Overview
- If you dissociate you might have symptoms such as not feeling connected to your own body or developing different identities.
- Dissociative disorder is a mental illness that affects the way you think. You may have the symptoms of dissociation, without having a dissociative disorder. You may have the symptoms of dissociation as part of another mental illness.
- There are lots of different causes of dissociative disorders.
- You may get talking therapies for dissociative disorders.
- You may be given medication that may help with symptoms of dissociation and dissociative disorder.
About
What is dissociation?
Many people will experience dissociation at some point in their lives. Lots of different things can cause you to dissociate. For example, you might dissociate when you are very stressed, or after something traumatic has happened to you. You might also have symptoms of dissociation as part of another mental illness like anxiety.
Some of the symptoms of dissociation include the following.
- You may forget about certain time periods, events and personal information.
- Feeling disconnected from your own body.
- Feeling disconnected from the world around you.
- You might not have a sense of who you are.
- You may have clear multiple identities.
- You may feel little or no physical pain.
You might have these symptoms for as long as the event that triggered them, or for a short time afterwards. This is called an episode.
For some people these symptoms can last for much longer. If you have a dissociative disorder you might experience these symptoms for long episodes or even constantly.
Types
What are the different types of dissociative disorder?
There are different types of dissociative disorder. There is more information on each of these below.
It‘s important to remember that you could have the symptoms of dissociation without a dissociative disorder. There is also a lot of disagreement among professionals over dissociative disorders.
What is dissociative amnesia?
If you have dissociative amnesia you might not remember things that have happened to you. This may relate to a stressful or traumatic event, but doesn’t have to.
In severe cases you might struggle to remember:
- who you are,
- what happened to you, or
- how you felt at the time of the trauma.
This isn’t the same as simply forgetting something. It is a memory ‘lapse’. This means you can’t access the memory at that time, but they are also not permanently lost.
With dissociative amnesia you might still engage with other people, such as holding conversations. You might also still remember other things and live a normal life. But you might also have flashbacks, unpleasant thoughts or nightmares about the things you struggle to remember.
You may have dissociative amnesia with dissociative fugue. This is where someone with dissociative amnesia travels or wanders somewhere else, related to the things they can’t remember. You may or may not have travelled on purpose.
What is dissociative identity disorder (DID)?
Dissociative identity disorder (DID) is sometimes called ‘Multiple Personality Disorder. But we have called it DID on this page.
If you have DID you might seem to have 2 or more different identities, called ‘alternate identities. These identities might take control at different times.
You might find that your behaviour changes depending on which identity has control. You might also have some difficulty remembering things that have happened as you switch between identities. Some people with DID are aware of their different identities, while others are not.
There is a lot of disagreement between researchers over the notion of DID.
We think of someone with DID as having different identities. But some researchers think that that these are actually different parts of one identity which aren’t working together properly.
They suggest that DID is caused by experiencing severe trauma over a long time in childhood. By experiencing trauma in childhood, you take on different identities and behaviours to protect yourself. As you grow up these behaviours become more fully formed until it looks like you have different identities. When in fact the different parts of your identity don’t work together properly.
What is other specified dissociative disorder?
With this diagnosis you might regularly have the symptoms of dissociation but not fit into any of the types.
A psychiatrist uses this diagnosis when they think the reason you dissociate is important.
The reasons they give include the following.
- You dissociate regularly and have done for a long time. You might dissociate in separate, regular episodes. Between these episodes you might not notice any changes.
- You have dissociation from coercion. This means someone else forced or persuaded you. For example, if you were brainwashed, or imprisoned for a long time.
- Your dissociation is acute. This means that your episode is short but severe. It might be because of one or more stressful events.
- You are in a dissociative trance. This means you have very little awareness of things happening around you. Or you might not respond to things and people around you because of trauma.
What is unspecified dissociative disorder?
This diagnosis is used where you dissociate but do not fit into a specific dissociative disorder.
Psychiatrists also use this diagnosis when they choose not to specify the reasons why you do not fit into a specific disorder.
Or if they don’t have enough information for a specific diagnosis. For example, after a first assessment in accident and emergency.
What are dissociative seizures?
Dissociative seizures are hard to get diagnosed. They are regularly wrongly diagnosed as epilepsy.
Dissociative disorders can also be known as non-epileptic attack disorder (NEAD).
It can be hard to tell the difference between a dissociative and epileptic seizure. An EEG can read epileptic seizures but can’t read dissociative seizures. An EEG is a test that detects electrical activity in your brain using small, metal discs attached to your scalp.
Dissociative seizures happen for psychological reasons not physical reasons.
What is depersonalisation/ derealisation disorder (DPDR)?
The feelings of depersonalisation and derealisation can be a symptom of other conditions. It has also been found among people with frontal lobe epilepsy and migraines.
But it can also be a disorder by itself. This means it is a ‘primary disorder’. There is some disagreement among professionals whether DPDR should be listed with the other dissociative disorders at all.
DPDR has some differences to other dissociative disorders. In DPDR you might not question your identity or have different identities at all. You may still be able to tell the difference between things around you. And there may be no symptoms of amnesia. Instead, with DPDR you might feel emotionally numb and questions what it feels like to live. We have explained this in more detail below.
You might have these feelings constantly rather than in episodes. It doesn’t have to have been caused by a traumatic or stressful event.
Many people think that this disorder might be more common than previously thought. This might be because of:
- a lack of information about it,
- patients who didn’t report their symptoms, and
- doctors who don’t know enough about it, meaning they underreport the condition.
With DPDR you might have symptoms of depersonalisation or derealisation or both.
Depersonalisation
With depersonalisation you might feel ‘cut off’ from yourself and your body, or like you are living in a dream. You may feel emotionally numb to memories and the things happening around you. It may feel like you are watching yourself live.
The experience of depersonalisation can be very difficult to put into words. You might say things like ‘I feel like I don’t exist anymore’ or ‘It’s as if I’m watching my life from behind glass’.
Derealisation
If you have derealisation you might feel cut off from the world around you. You might feel that things around you don’t feel real. Or they might seem foggy or lifeless.
Jane’s story
Causes
What causes dissociation?
There are different things that can cause you to dissociate. For example:
- traumatic events,
- difficult problems that cause stress, and
- difficult relationships.
Other researchers have suggested that the use of cannabis may sometimes be a cause of depersonalisation/ derealisation disorder (DPDR).
Treatment
How are dissociation and dissociative disorders treated?
Dissociation can be treated in lots of different ways. The type of treatment you get might depend on which type of disorder you have.
Can medications help?
At the moment, there are no medications for dissociative disorders themselves, although you may take medication for some symptoms.
If you have episodes of dissociation you might also have a condition such as depression or anxiety. Some medications could help with this. For example, antidepressants could be used for depressive symptoms and benzodiazepines for anxiety.
Benzodiazepines can be addictive and should be prescribed for a short period only. Benzodiazepines can make Dissociation worse.
You can find more information on:
What psychosocial treatments can help?
Talking therapies are usually recommended for dissociation. There are lots of different types of talking therapy. Different ones might be used for different dissociative disorders.
What is psychodynamic psychotherapy?
If you have DID, then your doctors may think about long-term relationally psychotherapy. This is a type of therapy where you talk about your relationships and thoughts. You might talk about your past. Your therapist can link the ways you think and act with things that have happened to you.
For DID, psychotherapy might be needed for a long time, with at least 1 session every week. This will depend on individual’s situations and on their ability and level to function, resources, support and motivation.
What is eye movement desensitisation and reprocessing (EMDR)?
DID may also be helped by eye-movement desensitisation and reprocessing (EMDR). In EMDR you make side-to-side eye movements while talking about the trauma that happened.
Doctors must be careful when using EMDR because it could make your DID worse if not done properly. But EMDR can have benefits when it is used along with other treatment. The type of EMDR used for DID is slightly different to other conditions. So, it is important that your doctor knows about your DID before you start EMDR.
What is cognitive behavioural therapy (CBT)?
Cognitive behavioural therapy (CBT) is another type of talking therapy. You will talk about the way your thoughts and feelings affect you. And how your behaviours may make this worse. You focus less on the past and try to change the way you think and behave.
Parts of CBT are recommended to treat DID, by helping you to change your thoughts and behaviours that come from the trauma.
A CBT approach has also been suggested for long-lasting DPDR. If you have DPDR you might often worry about your symptoms and think you have a serious mental illness or that something is wrong with your brain. CBT may help to change this way of thinking. By reducing your anxiety and depression that comes with this worrying, it may also reduce your symptoms of DPDR.
You can find more information about ‘Talking therapies’ by clicking here.
What treatment should I be offered?
In the UK, the National Institute of Health and Care Excellence (NICE) publish guidelines on physical and mental health conditions. These guidelines are a standard for NHS treatment. At the time of writing, there are no NICE guidelines on dissociation or dissociative disorders.
But this doesn’t mean you shouldn’t be offered treatment. If you think you are having any of these symptoms, then explain this to your GP. They may refer you to a psychiatrist.
You can find more about ‘GPs – What to expect from your doctor’ by clicking here.
What if I am not happy with my treatment?
If you aren’t happy with your treatment you can:
- ask for a second opinion,
- ask an advocate to help you speak to your doctor,
- contact the Patient Advice and Liaison Service (PALS), or
- make a complaint.
There is more information about these options below:
How do I ask for a second opinion?
If you aren’t happy with your diagnosis or treatment, speak to your doctor. If they don’t offer you any other treatment options, you can ask for a second opinion. This is where another doctor will assess you and suggest diagnoses or treatment. You don’t have a legal right to a second opinion, but your doctor might agree to one.
What is advocacy?
An advocate can help you understand your rights to treatment from the NHS. They can also help you be fully involved in decisions about your care. An advocate is separate from the NHS.
You can search online to see if there are any local advocacy services in your area. Or the Rethink Mental Illness Advice Service could search for you. You can find their details at the bottom of this page.
What is the Patient Advice and Liaison Service (PALS)?
The Patient Advice and Liaison Service (PALS) at your NHS trust can try and help you with any problems or issues you have. You can find your local PALS’ details at: www.nhs.uk/Service-Search/Patient-advice-and-liaison-services-(PALS)/LocationSearch/363.
How can I make a complaint?
If you aren’t happy with the way you have been treated, you can make a complaint. You have to make a complaint about the NHS within 12 months of what you want to complain about.
You can find more information about:
Self care & risks
What are self-care and management skills?
You can learn to manage your symptoms by looking after yourself at home. You will learn how to notice when you are becoming unwell and know what your triggers are.
Not all of the techniques here will work for everyone. It is important to try something that you enjoy and that you can commit to and that works for you.
Keeping a diary
You might find it helpful to keep a diary. You could write about how you felt over the day. Or you could write down goals that you want to achieve. You could use it as part of cognitive behavioural therapy (CBT).
Keeping a diary isn’t for everyone. If you have depersonalisation/derealisation disorder (DPDR) you might already spend a lot of time thinking about how other people see you. A diary may make you feel worse if it forces you to think about yourself. A diary can still help but talk to your GP or a counsellor first.
Grounding techniques
These techniques can be helpful for people who have been through trauma or who regularly dissociate. They can help to ‘ground’ you in the here and now. This may help when experiencing flashbacks.
Grounding works best when it is practiced regularly. Try practicing these things every day. There are different types of grounding techniques.
Using your surroundings
To use your surroundings, look around yourself. Focus on all the details of everything that is around you. Try describing this to yourself either out loud or silently in your head. Use all of your senses.
Using words
You could try positive words or phrases about yourself. For example, ‘I am strong’ or ‘I will succeed’. Write down a few things that are meaningful and positive for you. You could carry these around with you. Try reading them to yourself or aloud if your symptoms are bad.
Using images
This is similar to using your surroundings. Try thinking of a place that you feel peaceful and safe. This can be a real or imaginary place. If it is a real place, choose somewhere that is positive with no traumatic memories. Shut your eyes and imagine that place. Focus on all of the details and all of your senses.
Using posture
Try moving into a posture that makes you feel strong. This could be standing up with your shoulders back or relaxing your shoulders. Try different postures until you find one that works for you.
Using objects
Try choosing an object that is personal to you. You should try and pick something that only has positive memories attached to it. Carry it around with you and use it to remind yourself of who you are and where you are.
Relaxation
There are lots of different ways to relax. The important thing is to find something you enjoy doing. For example, cooking, reading or gardening. You might find that meditation or mindfulness helps.
Some relaxation techniques such as meditation and mindfulness may make some people feel worse. For example, if you have DPDR you might struggle with meditation. If this is the case, try and find something else that works for you. If you have CBT, you could tell the therapist. They could help you find something that works.
Exercise and diet
There are no specific exercises that can definitely help. But you could try jogging, swimming or just trying to walk more and something that suits your ability. Trying to eat more fresh fruits and vegetables can help. You could also try to reduce the amount of fat, salt and sugar you eat. Reducing the amount of caffeine, you drink can be helpful.
Sleep
If you don’t sleep enough your symptoms might feel worse. It can take a few weeks for you to get into better sleep habits. Here are some tips for helping you sleep.
- Sleep when you feel sleepy.
- Keep your bedroom as a place for only sleeping.
- If you are lying awake in bed for a long period, get up and move around for a while.
- Avoid taking naps during the day.
- Try not to have caffeine for a few hours before you go to bed.
- Make sure you get up at the same time every day. This can help you get into a regular routine.
You can find more information about ‘Complementary and alternative treatments’ by clicking here.
What risks and complications can dissociation cause?
Some people with a dissociative disorder may also have another mental health condition, such as anxiety or depression. This is called a ‘comorbid’ condition. In some cases, this can make your dissociative disorder harder in day to day life. However, all these conditions are manageable and treatable.
You can find more information on:
Carers, friends & family
What if I am a carer, friend or relative?
What support can I get?
If you are a carer, friend or family member of someone living with a dissociative disorder you can get support.
You can get peer support through carer support groups. You can search for local groups in your area on the following websites:
- Rethink Mental Illness: www.rethink.org
- Carers: Carers UK: www.carersuk.org
- Carers Trust: www.carers.org
If you need more practical support, you can ask your local authority for a carer’s assessment. You might be able to get support from your local authority.
As a carer you should be involved in decisions about your relative’s care planning. But you can only be involved if your relative agrees to this. If they don’t agree, their healthcare professionals can’t share information about them with you.
You can find out more information about:
- Carer’s assessment and support planning by clicking here.
- Confidentiality and information sharing – For carers, friends and relatives by clicking here.
- Benefits for carers by clicking here.
How can I supporting the person I care for?
You might find it easier to support someone with a dissociative disorder if you understand their symptoms, treatments and self-care options. You can use this to support and encourage them to get help and stay well.
You should also be aware of what you can do if you are worried about their mental state. Keep the details of their mental health team or GP handy and discuss a crisis plan with them.
You can find out more information about:
Further reading & Useful contacts
Caroline Spring
Online training on dissociation and Dissociative Identity Disorder, webinars and literature.
Website: www.carolynspring.com/
Clinic for Dissociative Studies
This organisation has lots of information on dissociative disorders on their website. They also provide care and treatment for dissociative disorders. They can accept referrals from the NHS. They offer general information about dissociative disorders but do not run a helpline.
Telephone: 020 7794 1655
Address: 35 Tottenham Lane, London, United Kingdom, N8 9BD
Email: [email protected]
Website: www.clinicds.co.uk
South London and Maudsley Trauma and Dissocation Service
A specialist outpatient assessment, consultation and treatment service. It’s for adults who are experiencing psychological difficulties following trauma and/or dissociative disorders. The only NHS specialist service offering treatment for people presenting with complex post-traumatic stress disorder (PTSD) and severe dissociative disorders. Referrals are accepted from GPs and senior clinicians. All referrals have to be approved and funded by the local clinical commissioning group (CCG).
Phone: 020 3228 2969
Email: [email protected]
Website: www.slam.nhs.uk/national-services/adult-services/trauma-and-dissociation-service
Dissociative Experiences Scale
Source: Dissociative Experiences Scale
A Screening Test for Dissociative Identity Disorder
This 28-question self-test has been developed as a screening test for Dissociative Identity Disorder, formerly known as Multiple Personality Disorder.
Completing this Psychological Screening Test
This questionnaire consists of twenty-eight questions about experiences that you may have in your daily life and asks how often you have these experiences. It is important, however, that your answers show how often these experiences happen to you when you are not under the influence of alcohol or drugs.
To answer the questions, please determine to what degree the experience described in the question applies to you and choose the button which corresponds to the percentage of the time you have the experience. The left of the scale, labelled ‘Never’, corresponds to 0% of the time, while the right of the scale, labelled ‘Always’, corresponds to 100% of the time; the range covers 0% to 100% in 10% increments.
Take the Quiz
Please note: This test will only be scored correctly if you answer each one of the questions. Please also check our disclaimer on psychological testing and our psychological testing privacy guarantee.
Try Online Counseling: Get Personally Matched
About Scoring this Psychological Questionnaire
When your quiz is scored, one of two different information pages will appear to describe the results for scores in your range, along with further details of how your score was computed. Roughly speaking, the higher the score, the more likely a diagnosis of a dissociative disorder.
This screening test for Dissociative Identity Disorder is scored by totalling the percentage answered for each question (from 0% to 100%) and then dividing by 28: this yields a score in the range of 0 to 100.
Generally speaking, the higher the DES score, the more likely it is that the person has DID. In a sample of 1,051 clinical subjects, however, only 17% of those scoring above 30 on the DES actually had DID.
The DES is not a diagnostic instrument. It is a screening instrument. High scores on the DES do not prove that a person has a dissociative disorder; they only suggest that clinical assessment for dissociation is warranted. People experiencing DID do sometimes have low scores, so a low score does not rule out DID. In fact, given that in most studies the average DES score for a DID person is in the 40s, with a standard deviation of about 20, roughly 15% of clinically diagnosed DID patients score below 20 on the DES.
The figure shown below plots DES scores (horizontal scale) versus the number of subjects (vertical scale) from a sample of 1055 people. For further information about the DES, its validity and scoring, please visit the Ross Institute.
Distribution of DES Scores in the General Population.
Additional Information
Flash Technique: A Useful Tool
Edited by Sophie Linder
I first heard of the Flash Technique (“FT”) in my Eye Movement, Desensitisation and Reprocessing (EMDR) therapy training by Dr. Philip Manfield in March 2019 in Oakland, California. EMDR is a form of psychotherapy that was developed by an American psychologist Francine Shapiro in the late 1980s. Since then, a lot of research has been conducted on the effectiveness of EMDR. Currently, EMDR is a widely recognized treatment for PTSD and other trauma-related conditions. The American Psychological Association (APA), among many others, lists EMDR as an evidence-based treatment for PTSD. EMDR consists of eight stages which typically require multiple psychotherapy sessions. During EMDR processing, the client focuses on the traumatic memory while eye movement, tapping, or another form of bilateral stimulation is used.
Dr. Manfield had developed FT in 2016, and was excited to share it with the class. Unlike EMDR, the Flash Technique does not require the client to commit to a lengthy process. It also does not require the client to focus on the traumatic memory for a long period of time. FT can be used as a part of EMDR treatment, or on its own. I thought that FT was an interesting tool, and I started using it along with the standard EMDR protocol. Sometimes I use FT to lower the intensity of the target, and then process the remainder by using traditional EMDR. My practice was both online and in person, and I used FT with both virtual and in-office clients. My interest in FT grew over time as I was getting good results, and I took the Flash Technique webinar in May 2020. In December 2020, I took the Advanced Flash Technique webinar. As of this writing, I have used FT with dozens of clients in the last two years. I have found it easy to use and very effective when working on a variety of disturbing memories and fears. It usually takes about 15 minutes to implement FT, making it very easy to fit into the standard 50 minute session.
The Flash Technique process starts with identifying a memory or fear, and ranking the level of disturbance that the client feels in that moment. The scale is 0–10, with 10 being the most disturbing. Next I ask the client to think of something fun or exciting that they can talk about for the next 10–15 minutes (i.e., a hobby, a pet, a movie, a trip). This is referred to as the Positive Engaging Focus (PEF). Then I demonstrate for the client how to cross their arms on their chest and tap on the arms (a butterfly hug). While they are tapping and talking about the PEF, I periodically ask them to blink several times in rapid succession. After five or so sets of blinks, I ask them to pause and touch on the target memory/fear. They rank the disturbance and tell me what they notice about the memory. Usually the target is less vivid and harder to pull up. Then we continue with the PEF and more blinking and tapping. Next we pull up the target again. This process continues until the target is no longer disturbing.
In the following session, usually a week later, I recheck the target memory or fear to see if there is still any disturbance. Some targets resolve in one session and the results hold over time. Typically, the easiest cases are single-incident traumas — an event that took place at one time and does not have any related memories. For example, someone who was in a car accident once and developed a fear of driving can usually process the incident in one session without any need for additional work. In other cases, usually when there are many related memories, it requires additional sessions of Flash or EMDR to fully resolve them. Multiple incidents can also be processed but may require additional sessions.
I should note that Flash, like EMDR, does not completely remove all fear. I would not want my clients to put themselves in unsafe situations following FT. Rather, FT and EMDR aim to take away the extreme disturbance associated with a traumatic event. The client still remembers that the event took place, and experiences a normal level of anxiety in appropriate situations. FT does not offer any superpowers or magical thinking. It removes the irrational fear so that the client can comfortably engage in everyday activities.
Here are several case examples in which I used FT:
Abbreviations:
FT = Flash Technique
SUDS = subjective units of distress (scale is 0–10, with 10 being most disturbing)
PEF = positive engaging focus (something positive and exciting that the client talks about during the sets)
Mugging
Della, a 33-year-old Caucasian female, was mugged seven years ago on the street. Since then, she had been unable to walk alone at night. She always had to have someone walk her places after it got dark, or she avoided going out altogether. She stated, “I want to be able to walk alone at night if I need to.” Della lived in a safe suburb and did not have an urgent need to go anywhere at night. More recently, Della’s company offered to relocate her to Paris. Della was excited about the opportunity, but realized that she needed to work on this fear if she was going to move to a big city.
We discussed the mugging in more detail. The incident happened when she was in college. She was studying late at the library, and drove home to her apartment at around 2 a.m. She parked her car in a garage a block away from her apartment. As she was walking home, three people came up behind her. They kicked her to the ground, grabbed her backpack containing a laptop, and drove away. When asked to rank the disturbance associated with this memory, Della stated it was a 9 on the 0–10 scale. For Flash, we chose Paris as her positive engaging focus. “I’m excited to move there,” Della said. After five sets of Flash which took about 10 minutes, Della ranked the disturbance at 1 before the session ended.
Two weeks later, Della reported that she had chosen a safe area in her suburb as a test for an evening walk. She walked alone at around 8 p.m. Della stated, “This is something I haven’t been able to do since the mugging seven years ago.” She said that it felt good to walk around and look at the lights. In the past, she would have felt very anxious at the thought of walking alone at night. “This time, I didn’t have any physical symptoms,” said Della. She described that she did feel a little nervous, ranking the SUDS at 1–2. However, it felt like a normal amount of anxiety compared to the paralyzing fear she had experienced previously. She felt good about the outcome. “I wanted to be able to walk alone at night if I had to, and now I can do that,” Della remarked.
Fear of being alone
Danielle, a 37-year-old mixed race Caucasian and Asian-American woman, sought therapy with me for anxiety and depression in July 2020. Danielle shared that her “number one fear” was of being alone, and one day, dying alone. Danielle ranked the SUD at a 10. One of the contributing factors to this fear was Danielle’s current relationship with her boyfriend of a couple years. Danielle wanted to move in together, but her boyfriend decided that he wasn’t ready, and instead rented a one-bedroom apartment in another city. Danielle stayed in her one-bedroom apartment where she was living by herself. In addition, her best friend had moved away recently. “I am afraid I will always live alone in an apartment.” The fear was exacerbated by the COVID-19 pandemic and resulting isolation.
To me, the fear seemed largely irrational as Danielle was a very attractive woman with an impressive educational background and a successful career. She had a great personality, was easy to talk to, and had interesting thoughts and ideas. We decided to use Flash on this fear, and we used food as the PEF. After two sets, SUD decreased from 10 to 7–8. When I asked Danielle what was different about the target, she stated, “I’m not in the visual anymore.” After two more sets, Danielle reported, “I feel less sad.” SUD = 6.
A few weeks later, we checked on her fear of being alone. Danielle ranked the disturbance at 3–4. I asked her to explain the source of her disturbance. Danielle replied, “My grandma died alone in a nursing home. She was a prom queen in high school–I have a picture of her. By the time she died, she was decrepit and had bad teeth. I feel guilty that I didn’t visit her.” We decided to continue with Flash. For PEF, Danielle chose comics and graphic novels. After two sets, she reported that the image had faded. “I feel guilty we weren’t close,” she said. Danielle cried and reported the disturbance at 6–7. She pointed out that the fear of being alone on its own was at 2. After the third set, she stated, “The strong emotions about my grandma have dissipated,” and was no longer crying. After the fourth set, she reported, “I feel less afraid of the memory.” For grandma, SUD = 1; for the fear, SUD = 0. She added, “There are things I can do in my lifetime.” I guided Danielle in instilling this positive belief using slow self-tapping. By the end of the session, Danielle was smiling.
The following week, I asked Danielle about the fear of being alone. She stated, “I used to think about it throughout the day, every day, but now I don’t think about it.” She said it felt like 0–1 now. Danielle added, “I am more focused on what I can do now to create a better future for myself.” She reported that she started to organize her finances this past week. She also engaged with new and old friends with the goal of having deeper friendships. I asked Danielle what she thought of the Flash technique, and she said she found it helpful.
Dad’s Addiction Issues
Claudia, a 31-year-old African-American female sought therapy with me in January 2021 to work through family issues. Claudia achieved a lot in her life; she put herself through undergraduate and graduate school where she studied biochemistry, and landed her dream job where she was succeeding. She was happily married to a wonderful young man. However, she struggled with anxiety, especially around her father’s past and current substance abuse issues. Claudia explained that her father was an active alcoholic and has abused cocaine on occasion since she was a child. I asked her to write down her 10 worst memories. Six of her 10 memories involved her father. We noted how disturbing they felt as we went over them.
In our next session, we targeted the first bad memory which was “Dad being high at dinner.” Claudia was 14 at the time. She rated the disturbance associated with the memory (SUD) at 6. Claudia picked her honeymoon as her PEF. With each set of Flash, the disturbance associated with the memory went down by 0.5–1. After eight sets, Claudia reported that the memory did not bother her anymore. “I can’t see my dad’s face anymore,” she said. In the following session, we checked the memory and the disturbance was back at 3. For her PEF this time, Claudia chose her wedding. After two sets, she reported that the event was “hard to recall.” The memory no longer had a hold on her. “I feel indifferent,” she said. The positive belief was “I’m not at fault.” I asked Claudia to close her eyes and play the event in her mind while repeating the words “I am not at fault” as she tapped slowly.
Next I asked Claudia to imagine a folder named “Dad’s addiction issues.” I asked her how disturbing it felt to think of the folder, and Claudia said 5–6. For her PEF, Claudia decided to continue talking about her wedding. After two sets of Flash, she reported that, “Specific memories are hard to pull up.” After two more sets, she reported there was no disturbance. We checked each Dad-related memory, and the disturbance was 0–1 for each. In our next session, I asked about the memory of dad being high at dinner. Claudia reported that she felt 0 disturbance. I asked if there was anything else that felt disturbing to her regarding her dad’s addiction. She replied, “Yes, I am worried about his health. He continues to drink, and he could have a stroke and die early.” This fear felt like a 2 to her.
I decided to use the standard EMDR protocol for this fear. The negative belief was “I’m not in control”; the positive belief was “I can handle whatever happens.” We worked through several channels. One aspect that was particularly painful for Claudia was that her brother was very close to their dad. She cried when she thought about the pain her brother would feel if her father had a stroke in the near future. I used several cognitive interweaves which Claudia found helpful: “You’ve done your part,” and “We don’t know when your dad will pass; he could live for a long time despite his addiction issues.” After several sets, Claudia realized that she would be there for her brother when her dad passes away, which she found to be calming.
By the end of the session, the fear of her father’s early death was no longer impacting her. “If it happens, I can handle it,” Claudia stated. We conducted a body scan which revealed that the pit in her stomach from earlier in the session went away. Claudia reported that she felt good about the work we had done, and at peace regarding her father’s addiction. She no longer felt that it was her fault, or that she should be doing something to force him to stop (which she had tried in the past without success). She felt free to enjoy her relationship with her father as it is today, and let go of fear of the future.
Fear of Cats
Georgia, a professional Hispanic woman in her late 20s, had an extreme fear of cats which made her life difficult. She couldn’t visit her best friend, Zoe, because Zoe had a cat at home. When Georgia saw cats on the street, she felt apprehensive and had to walk away immediately. Georgia was single and actively dating, but had to exclude any potential partners who lived with a cat.
It turned out that Georgia had a traumatic experience with cats as a child. She explained, “It was during my first piano exam at my instructor’s house. I was nervously waiting for my turn to play, and four cats came up to me and scared me.” The cats appeared suddenly and came up to her from behind. Georgia estimated her age to be seven years old at the time. When I asked her how disturbing this memory felt now, she ranked it a 6 on the 0–10 scale. We decided to process this memory with the Flash Technique. We used Georgia’s favorite TV dating show as a PEF. After two sets, Georgia remembered that during a sleepover in high school, a cat jumped on her bed which was scary. After one more set, the fear was 0. This process took about 10 minutes.
In our next session a week later, Georgia reported that the memory of the four cats at the piano exam was not disturbing (SUD=0). I asked Georgia to imagine visiting Zoe and her cat. She reported there was no disturbance. I asked Georgia to pull up a picture of a cat online, and she reported 0 disturbance. Then I asked her to search for a video on YouTube of a cat attacking a person. She watched the video in session and her facial expression was unremarkable; again there was no disturbance. After a few weeks, Georgia reported that the piano exam memory did not produce any disturbance. Picturing cats was not disturbing. Due to the COVID-19 quarantine, she had not had a chance to visit any friends with cats yet.
After a few more weeks, Georgia reported that the fear of cats was 0. She added, “There are some cats that walk on the fence in my backyard. I used to find it really irritating and distracting. I would try to scare them off. Every other weekend I would spray the fence with vinegar to keep them away. It didn’t work! They still came back. Now it doesn’t bother me. The other day I even thought the cat was cute.” Georgia explained that she did not fall in love with cats or anything like that, but the fear was no longer there. She felt neutral towards them which allowed her to live her life with more peace. This result was well worth the 10 minutes that she spent trying out the Flash technique.
Aside from the above examples, I have successfully used FT with other clients, focusing on a variety of negative memories and fears. Some examples include a parent’s suicide, childhood bullying, extreme fear of bugs, chronic pain and fear of becoming disabled, fear of contracting COVID-19, sexual assult, car accident/fear of driving, near drowning/fear of swimming. In some cases, the problem resolved after 15 minutes of FT with no resurgence. In other cases, FT provided some benefit but additional EMDR work was required to fully re-process the event and maintain results over time. To date, I haven’t had any negative experiences with FT. Most clients have found FT to be helpful and enjoyable.
It should be noted that FT, like any other therapeutic intervention, may not be effective for every client or issue. Clients should be aware of potential risks and limitations of FT before starting therapeutic treatment.
About the author: Annia Raysberg, MFT is a therapist in private practice living in Castro Valley, CA. She is currently working with clients via video. For more information, please visit AnniaRaysberg.com.
Client’s names and other identifying details have been changed. Written permission has been received from clients.
Articles on Flash:
Manfield, P., Lovett, J., Engel, L., & Manfield, D. (2017). Use of the flash technique in EMDR therapy: Four case examples. Journal of EMDR Practice and Research, 11(4), 195–205. http://dx.doi.org/10.1891/1933-3196.11.4.195.
EMDR and The Flash Technique: A match made in heaven? — EMDR Therapy Quarterly (emdrassociation.org.uk)
Shebini, N. (2019). Flash technique for safe desensitization of memories and fusion of parts in DID: Modifications and resourcing strategies. Oct 2019, Frontiers of the psychotherapy of trauma and dissociation Vol 3 3(2):151–164 2019 ISSN 2523–5117 print/ 2523–5125 online
Wong, Sik-Lam. (2019). Flash technique group protocol for highly dissociative clients in a homeless shelter: A clinical report. Journal of EMDR Practice and Research, 13(1), 20–31. http://dx.doi.org/10.1891/1933-3196.13.1.20
About EMDR Therapy

Eye Movement Desensitization and Reprocessing (EMDR) therapy is an extensively researched, effective psychotherapy method proven to help people recover from trauma and other distressing life experiences, including PTSD, anxiety, depression, and panic disorders.
The American Psychiatric Association, the American Psychological Association, the International Society for Traumatic Stress Studies, the Substance Abuse and Mental Health Services Administration, the U.S. Dept. of Veterans Affairs/Dept. of Defense, The Cochrane Database of Systematic Reviews, and the World Health Organization among many other national and international organizations recognize EMDR therapy as an effective treatment. More specific information on treatment guidelines can be found on our EMDR and PTSD page.

How is EMDR therapy different from other therapies?
EMDR therapy does not require talking in detail about the distressing issue or
completing homework between sessions. EMDR therapy, rather than focusing on changing the
emotions, thoughts, or behaviors resulting from the distressing issue, allows the brain to
resume its natural healing process.
EMDR therapy is designed to resolve unprocessed traumatic memories in the brain. For
many clients, EMDR therapy can be completed in fewer sessions than other
psychotherapies.

How does EMDR therapy affect the brain?
Our brains have a natural way to recover from traumatic memories and events. This process involves communication between the amygdala (the alarm signal for stressful events), the hippocampus (which assists with learning, including memories about safety and danger), and the prefrontal cortex (which analyzes and controls behavior and emotion). While many times traumatic experiences can be managed and resolved spontaneously, they may not be processed without help.
Stress responses are part of our natural fight, flight, or freeze instincts. When distress from a disturbing event remains, the upsetting images, thoughts, and emotions may create feelings of overwhelm, of being back in that moment, or of being “frozen in time.” EMDR therapy helps the brain process these memories, and allows normal healing to resume. The experience is still remembered, but the fight, flight, or freeze response from the original event is resolved.

Who can benefit from EMDR therapy?
EMDR therapy helps children and adults of all ages. Therapists use EMDR therapy to address a wide range of challenges:
- Anxiety, panic attacks, and phobias
- Chronic Illness and medical issues
- Depression and bipolar disorders
- Dissociative disorders
- Eating disorders
- Grief and loss
- Pain
- Performance anxiety
- Personality disorders
- PTSD and other trauma and stress-related issues
- Sexual assault
- Sleep disturbance
- Substance abuse and addiction
- Violence and abuse

Can EMDR therapy be done without a trained EMDR therapist?
EMDR therapy is a mental health intervention. As such, it should only be offered by properly trained and licensed mental health clinicians. EMDRIA does not condone or support indiscriminate uses of EMDR therapy such as “do-it-yourself” virtual therapy.
EMDR Therapy is a Recognized Effective Treatment for PTSD
Anyone can experience intense trauma. EMDR therapy is widely considered one of the best treatments for post traumatic stress disorder (PTSD) and it has been endorsed as an effective therapy by many organizations.

Complex PTSD Symptoms And Treatment | Betterhelp
Source: Complex PTSD Symptoms And Treatment | Betterhelp
By: Darby Faubion
Updated January 08, 2021
Medically Reviewed By: Melinda Santa
If you or someone you love is currentlyaffected by Complex PTSD, it can feel like you don’t know what else to do. You might feel stuck or alone in your struggle. No matter what you’re experiencing right now or in the past, there are tools to help you move forward to a life that feels lighter, happier, and healthier. The fact that you’re here right now looking for answer is a great indicator that hope is not lost. Taking the courageous step to investigate and pursue treatment for managing your symptoms is a victory.
Post-traumatic stress disorder (PTSD) is a trauma-based mental illness. It manifests in many ways and can look very different. Often it causes severe anxiety around certain triggers, a sense of jumpiness, distressing nightmares, and persistent feelings and symptoms of distress. Anyone who has experienced, witnessed or repeatedly been exposed to details of atraumatic event may develop PTSD in response. In particular, individuals who have experienced repeated or ongoing trauma may be at risk for developing Complex Post-Traumatic Stress Disorder (C-PTSD).
While PTSD may develop after a single incident, C-PTSD is a group of complex symptoms that result from long-term traumatic events. Examples of ongoing trauma include long-term physical or sexual abuse, ongoing domestic violence, being a prisoner of war, or being a victim of commercial sexual abuse, including trafficking or prostitution. C-PTSD is thought to be more severe in those who experienced traumatic events for a long time, at a young age, were alone in the experience, or the experience was enacted by a caregiver, especially one they are still in contact with.
In this article, we’ll look closer at the symptoms, which bear similarity to the symptoms of PTSD, and treatment for Complex PTSD.

This website is owned and operated by BetterHelp, who receives all fees associated with the platform.
Source: unsplash.com
Symptoms of C-PTSD
Complex Post-traumatic Stress Disorder usually encompasses the following PTSD symptoms:
- Avoidance
- Avoiding places, people, or situations that remind someone of the traumatizing event(s)
- Avoiding thoughts, memories, and feelings of the traumatizing event(s)
- Re-experiencing
- Nightmares of the traumatizing event(s)
- Distressing flashbacks of the traumatizing events(s)
- Frightening thoughts about the traumatizing event
- Mood and Cognition
- Distorted or misplaced thoughts of guilt or blame
- Negative thoughts about the world or oneself, including a sense of hopelessness or worthlessness.
- Loss of interest in hobbies and activities
- Problems remembering specific events relating to or surrounding the period of trauma
- Arousal and Reactivity
- Sleeping problems, including waking early, insomnia, and oversleeping
- Feeling stressed, on edge, or irritable
- Feeling jumpy or startlingeasily
- Experiencing outbursts of anger

Source: pexels.com
In addition to the list above, people suffering from C-PTSD may also experience the following symptoms:
- Difficulty relating to others
- An ongoing search for a rescuer
- Distrust of others
- Isolating oneself from relationships, even close ones
- Avoiding close relationships altogether
- Difficulty regulating emotions
- Outbursts of anger
- Persistent sadness and depression
- Suicidal thoughts. If you are experiencing thoughts of suicide, reach out for help immediately. The National Suicide Prevention Lifeline can be reached at 1-800-273-8255.
- Cognitive difficulties
- Problems with memory (forgetting traumatic events or details surrounding them)
- Feeling disassociated or detached from emotions and their sense of self
- Reliving traumatic events persistently
- Difficulty with self-perception
- Perceiving oneself as guilty and unworthy of help
- An overwhelming sense of shame
- Perceiving themselves as helpless
- Feeling different from others
- Preoccupation with the perpetrator/perpetrators
- Preoccupation with revenge
- Preoccupation with one’s relationship to the perpetrator
- Attributing power to the perpetrator
- Damage to one’s belief system
- Lack of faith
- Inability to feel hopeful
- Overwhelming feelings of despair
Because children and teenagers do not have the same coping mechanisms as adults, the symptoms they exhibit after prolonged traumatic events may be a little bit different. For example, children who are six years old or younger may also experience the following symptoms:
- Bedwetting after they have learned to use the toilet
- Acting out the traumatic event while playing
- Loss of speech
- Clinging to a parent or other adult; fear of being separated from them
Older children and teens experience many of the same symptoms as adults, although sometimes also experience the following symptoms of C-PTSD:
- Disrespectful or destructive behavior
- Misplaced guilt over not being able to prevent death or injury
- Feelings of or a preoccupation with revenge

Standard behavioral therapies teach coping mechanisms and help individuals to recognize and change their negative thoughts and behaviors. This type of therapy also focuses on addressing symptoms as they arise, rather than ignoring them or trying to push through them to something more positive.
At times, it may be necessary or helpful to use medications to manage C-PTSD symptoms. Some medication regimens may include antidepressants, anti-anxiety medications, and sleep aids.
Antidepressants help to relieve some negative mood symptoms, such as excessive guilt, shame, and blame. Alternatively, anti-anxiety medications are used to help relieve the symptoms of fear, worry, and stress that often accompany a diagnosis of C-PTSD.
Another therapeutic method known as cognitive restructuring therapy focuses on dealing with how the traumatic event occurred and helping the patient understand theirthought processes around the event. For many, self-blame, guilt, and shame are major symptoms of the diagnosis, so restructuring therapy helps put traumatic events in perspective. It works to ease these feelings by looking at the reality of the situation.

Source: pexels.com
Exposure therapy is a type of psychotherapy that exposes individuals to the trauma they once experienced in a safe way. During exposure therapy, individuals learn to face their fears, recognize their own ability to cope with it, and exert control over their reactions and impulses. This therapy often works for people who have severe symptoms of anxiety related to their traumatic experiences. It may be a step taken later on in a patient’s treatment plan.
There Is Help
The fear of rejection that often accompanies a C-PTSD diagnosis may cause some people to be apprehensive about seeking help. The benefits of talking with someone who can help you navigate the healing process is crucial.
There are many options for talking with a counselor or therapist. Some people prefer to meet in-person in a controlled setting, like a therapist’s office. It provides a safe place to explore feelings and learn new tools. Others may prefer to have more control over when and where they communicate with a counselor. In these instances, online counseling is a great option.
BetterHelp,an online counseling platform, can connect you with experienced counselors, doctors, and social workers who can help you address Complex Post-Traumatic Stress Disorder and any other mental health issues you may be facing. Their goal is to provide professional help to anyone who needs assistance navigating life’s difficulties.Online counseling for battling symptoms related to C-PTSD, like depression and anxiety, has been shown to be just as effective as in-person sessions. A study looking at 318 BetterHelp users found that those users experienced a significant reduction in depressive symptoms in just 3 months of sessions.
Online counseling can be a great, straight forward to begin receiving help today. With no waiting around for an open spot in your local counselor’s office, online counseling can begin as soon as you’re ready, whether via messaging or phone calls or video chats. Plus, BetterHelp’s service is completely confidential, making sure your information stays safe and private.
Below you’ll find some reviews of BetterHelp counselors from people experiencing similar issues.
Counselor Reviews
“Ted is an example of what a person is gifted to do!!! Has given me direction to go forward with complex PTSD. It’s been a productive year and looking to more growth.”
“Dr. Cooley was able to identify my needs and address appropriate therapy. I no longer have PTSD events that are not manageable. He has given me tools and resources to deal with my issues. I became brave enough to make positive change in my life and found I could experience joy and genuine love.”
Conclusion
Dealing with any kind of trauma can feel overwhelming, but help is available. If you’re affected by complex post-traumatic stress disorder, you can learn tools to work through your trauma and regain your sense of power and identity. With help from a qualified therapist, it’s possible to gaincoping mechanisms to lead a healthier life. Take the first step today.
Previous Article
Do You Suffer From Survivor’s Guilt?
Next Article
Common Treatments For PTSD Nightmares
How EMDR Helped Me Find Healing in a Most Daunting Year

In 1987, psychologist Francine Shapiro, Ph.D., noticed that moving her eyes from side to side while contemplating difficult thoughts improved her mood. Intrigued, she went on to research and develop EMDR. Shapiro suggests there are approximately 10 or 20 unprocessed memories responsible for most of the pain in our lives. The efficacy of EMDR therapy in the treatment of PTSD has since been well established, as evidenced by the results of over 30 positive randomized controlled studies over the past three decades. Such findings led the World Health Organization to state in 2013 that Trauma Focused Cognitive Behavioral Therapy (TF-CBT) and EMDR are the only psychotherapy modalities recommended in the treatment of those diagnosed with PTSD.
EMDR aims to process trauma in a more detached way than simply retelling the stories, which can be too emotionally intense. It works in eight phases: history taking, client preparation, assessment, desensitization, installation, body scan, closure, and reevaluation of treatment effect. The therapist will first learn about the client’s history, while also helping them to create a sense of safety in the body. From here, key memories are identified and reprocessed. Bilateral stimulation is used at certain points in the therapy, while working through painful memories. Some of the methods are eye movement from side to side (guided by the therapist’s hand), alternating electrical pulses from a therapulse device held in both palms, headphones with alternating tones beeping from ear to ear, or glasses with flashing lights. This is based on the client’s individual preference and comfort level.
Once the memories are reprocessed in this way, your brain develops new neural pathways. According to Michael G. Quirke, an EMDR therapist in San Francisco, “a brain that can change is capable of putting to rest old feelings, learning new ways of responding, and interpreting thoughts and feelings differently. The way you think, feel, and respond as a result of trauma can be rewritten and healing can become more possible.” This process in the brain is called neuroplasticity, and ultimately it promotes the formation of new, positive associations with the original event, such as “the risk of harm has passed and I am now safe.” The brain can heal from psychological trauma, much as the body recovers from physical trauma, allowing someone to act from a place of self-awareness rather than conditioning.
O’Shea Brown and I used a therapulse while I worked through my memories, starting slowly to build up to more traumatic thoughts. Before and after EMDR she asked me to rate, from one to 10, how distressing my main negative belief was from the trauma we discussed. With each session the numbers got lower, and I felt encouraged to go further. It was like shining a flashlight into a dark closet to find that the monsters I placed there were no longer present, and therefore not threatening to me. When COVID-19 hit and in-person therapy abruptly ended, we decided to continue with virtual EMDR (vEMDR). I was soon to discover that COVID-19 presented more than a few challenges for both therapist and client.
The spread of the virus and the isolation that followed has created mental health issues nationwide. For people with complex post-traumatic stress disorder, or C-PTSD (the experience of multiple and/or prolonged traumatic events rather than a single incident event), the pandemic had the power to heighten the risk of re-traumatization and exacerbate symptoms. “The abrupt loss of social norms has the potential to activate hypervigilance in many trauma survivors, while also creating a large-scale sense of uncertainty that is characteristic of a global pandemic,” O’Shea Brown explained. I could relate: All of the major pillars of my life began to come apart at the same time. My mother got out of a rehab facility from a fractured pelvis only a few weeks before COVID-19 hit, and the last time I saw her she was in a hospital bed. Then my mother-in-law passed away. My husband retired from a 20-year career as a homicide detective the first week of March and we went for a short visit to Tennessee to be with his father. Suddenly a few days trip became a six-month quarantine, followed by a move out of New York City and to the South. My oldest sister passed away in the summer and I didn’t have a chance to see her or to say goodbye. I needed to cling to the positive aspects of my old life, so EMDR therapy felt more essential than ever.
Since its inception, EMDR has been understood by both therapists and clients as a powerful vehicle for processing traumatic experiences, but only when the client has achieved stabilization. “Changes to treatment which ordinarily would be carefully cocreated and discussed over weeks or months were hastily made as this large-scale crisis began unfolding precipitously,” O’Shea Brown reflected. “Teletherapy is one potential alternative to in-person sessions; however, teletherapy is a privilege reserved only for those who can afford a phone, stable internet connection, and/or a laptop, as well as a place of solitude where they can confidentially and safely process their emotions.” For me, finding a place of solitude became nearly impossible while quarantined in a home for two that now housed four people and two dogs. Technological difficulties made things even more frustrating. Trying to talk about traumatic events when my dogs were barking, people were talking right outside my door, and the EMDR app on my phone was glitchy only heightened my anxiety. On one occasion, I was processing a charged memory when I saw the meter man right outside my window. I felt exposed. I missed the in-person sessions I had with my therapist. It can be difficult to focus without the safe protective cocoon of the therapy office.
Achieving a stable state during such turbulent times has been difficult, if not impossible. There is a shared energy and a deep connection that can happen when you are only a few feet apart from another person. During our in-office time, I felt a sense of safety and calm that I no longer feel with virtual sessions. It was easier to let down my guard and be fully present in the moment when we were able to share space.
I’ve had to remind myself that healing is a journey, with good days and bad days. Sometimes we can proactively reprocess painful memories and sometimes I just need to respond to the current chaos of life. There are days when I cannot center myself and the “noise” in my head and body are too overwhelming, so my therapist is gentle as we cocreate an experience that feels safe. We discuss the present rather than delving deeper into the past, and she helps me to utilize some of the inner resources I’ve developed through EMDR. On good days, when I can relax and tune in, I see a light at the end of the tunnel and a future where EMDR can help me to unburden myself of past trauma and access my own innate healing wisdom.
The Butterfly Hug
The Butterfly Hug is a form of bilateral stimulation that can be used as a grounding technique.The process is simple and can be done in any situation. It can help bring you back to the present moment and calm your emotional state.
AFFIRMATIONS: 15 Phrases to Repeat When You Don’t Feel Good Enough
8. I am thankful that my life is filled with wonderful things.
A total transformation in attitude begins with gratitude. When we are grateful for every wonderful thing in life, we are able to feel more fulfilled.
You’ll find yourself growing in self esteem when you understand how blessed you are.
9. My thoughts are positive, healthy, and loving. These thoughts eventually become my life experiences.
We are the only ones that have total control over our thoughts. So, it is essential that we choose to entertain thoughts that are filled with love and positivity.
10. I am a solution-maker. I am driven to see every problem as an opportunity for growth.
Life isn’t easy, but in the grand scheme of things, there is no problem that we can’t solve. Whether we find a solution that works out or doesn’t work, every moment gives us the chance to learn more about ourselves and the world.
11. Though I may be a single person, I’m not alone. I am always supported by the universe in ways I see and do not see.
Though at times we may feel alone, the universe is always rooting us on. Though the universe is often working in mysterious ways, it is always working towards our good.
12. I have a past but I’m not my past. I live in each moment so I can enjoy life to the fullest.
We all have good and bad in our past. Choosing to embrace every moment that we have is an important part in moving on from our past and truly being in the moment.
13. I am constantly changing and can grow into whomever and whatever I want.
We all are growing into the person we were always meant to become. Though other people may try to influence us to grow in certain ways, only we are in control of who we want to be.
14. I am the only person responsible for deciding what to do with my life.
Our lot in life is our choice–no one can tell us any different. We must do what makes us happy and what brings us joy.
15. When I choose to prioritize myself and my desires, I am not selfish for doing so.
Self care is all about recognizing our own needs. Doing this is the only way we can bring joy to other people’s lives. For this reason, taking care of ourselves should be our highest priority.
16. I have a choice with each moment to choose positivity or negativity. I always choose positivity, no matter what is happening in my life.
We don’t have to have negative experiences, thoughts, or mindsets. By recognizing the choices we make in each moment, we can transform our lives to be filled with positivity.
17. I am a flexible person that enjoys new experiences and meeting new people.
Life is all about charging into the unknown confidently and unafraid. We all have a certain flexibility and strength inside us that allows us to enjoy new experiences.
18. I am a strong person and I am always aware of this. I always choose to walk in confidence.
We must never let anyone diminish our strength. We are stronger than we know and must always be aware of this.
Best Practices for Living Out Daily Affirmations
To make the most of these affirmations, we must make a habit of living them out through the following means:
1. Write Out Negative Thoughts
We all have negative thoughts every now and then. To counteract these thoughts, it helps to make a list with all our negative qualities. This list can include any criticisms that other people have spoken over us. Oftentimes, we hold all this negativity inside without realizing it.
During this part, we must remember that we all have flaws. It is our responsibility to never hold onto these negative things. Instead we must let them go.
2. Counter Each Negative Point with an Affirmation
Now that we have a list of negative qualities and self-judgements, it’s time to counter them with the positive affirmations. The above affirmations are a great source of inspiration for the kind of statements we must use to overcome any negativity.
For example, a negative criticism like “I never do anything right” should be countered with the statement “I am capable of achieving everything I put my mind to.”
The more confident and self-assured the affirmations, the better.
3. Repeat the Affirmations Each Day
The real shift in thinking comes when repeating the affirmations becomes second nature. Start by scheduling time to repeat each affirmation at least three times each day.
The best time to repeat these affirmations is in the mirror. That way, the affirmations will really sink in as we say them directly to ourselves.
In addition to repeating these affirmations, writing them out is also helpful. Writing these words over and over in a mindfulness journal will help us to keep them in mind.
4. Anchor Every Affirmation
Every affirmation should be “anchored” to a specific place in the body. When we read these aloud, we must place our hands over the area that was referenced in the initial negative statement.
Similarly, we can anchor the affirmations by “breathing” into them. Every time we say an affirmation, we must breathe in the positivity and exhale the negativity.
5. Ask a Friend to Repeat the Affirmations
Boost your self esteem by asking a trusted friend or family member to speak these affirmations to you. This will have a profound effect on your psyche. Simply having someone speak this positivity over you is a powerful act.
Final Thoughts on Positive Affirmations
Using positive affirmations in our daily lives allows us to completely transform our state of mind, mood, and our goals in life. To really harness the power of positive affirmations, it is important for us to undo the damage caused by negative beliefs. By using positive affirmations to counteract these thoughts, we are working to create an entirely new reality for ourselves.
This mindfulness practice allows for a total revolution in self esteem. While we can’t escape negative things in life, we can change how we react to things and how we treat ourselves. By choosing positivity, we are on the way to becoming the best versions of ourselves and living the life we’ve always wanted.
I was abused as a child. Should I tell my mother? | Family | The Guardian
Source: I was abused as a child. Should I tell my mother? | Family | The Guardian
You were failed by the adults around you, says Annalisa Barbieri, and must now put yourself first
My childhood was lonely and frightening. A female friend lived with my father, mother, brother and I when we were children. She had an affair with my father and was a bully towards me and my brother when nobody else was around. The affair was not hidden from me and left me very stressed, and feeling guilty at five years old.
Around this time she suffocated me with a pillow and later stuffed me in a pillowcase. She also tried to drown me in the bath. I can still remember pretending to be dead to stop the suffocation. For nearly two years I lived in fear and guilt. Later, the affair came out. Dad left and died soon after.
My father was loving and caring but, sadly, not the best husband. He was a flawed man, but not a bad one. My mother is a good mum, but hard to talk to about the past. She’s never discussed her own past much, and I’ve learned more about it from other family members.
I was later also sexually abused by a babysitter. This I don’t remember as much; I think my brain does not want me to know. I have blanks in my past that I just can’t remember, which is more frightening than a comfort.
I told my brother, which was hard (we aren’t close) and he wants me to tell my mum. I’m in my 30s now, so how do I tell her I kept my abuse from her? Is it the right thing to do? I don’t want to take my abusers to court. I doubt I would get justice.
The reason I asked my brother was that I wanted to know if anything had happened to him. The question plagued me for so long. He wasn’t abused, thank God.
What do I do? I feel lost. Do I tell my mum what happened? It won’t change the abuse.
You have been horribly abused by the woman who tried to kill you, and your babysitter. And despite all that has happened to you, here you are caring about your brother, worrying about how you kept the abuse from your mum. Nothing that happened was your fault. You were failed and harmed by all the adults around you. I’m so sorry.
I wondered why you told and asked your brother now, and what else is happening in your life at the moment? Often survivors of emotional, physical and sexual abuse reach a safe place and can look back at what happened – maybe this resonates for you? Or maybe you are at the stage of life where you might be thinking of having children of your own?
I talked to Joanne Stubley, a consultant psychiatrist and a specialist in trauma. She was impressed with your ability to recognise the failings in your parents and not just “see things in black and white, which is what often happens with trauma”. She said: “The big question is whether you should tell your mum or not: but that didn’t seem to be coming from you, but rather from your brother.”
She felt that, before you do anything, you might want to work on “putting all of this together”. While you remember the assaults by the family friend clearly, Stubley thought you described the process of dissociation in relation to the babysitter very accurately when you explained that maybe your brain didn’t want you to remember.
We both agreed that you need to put yourself at the centre of anything you do next. I can understand you wanting to talk to your mother, but I am not sure if she is the best person for you to speak to right now. Stubley wanted you to be very sure – or as sure as you can be – of what you do from now on, so you are not motivated by revenge or anger, or even wanting to save anyone else. This is important because you need to be careful not to repeat what happened to you before: people not noticing, not listening, not protecting you. If that were to happen again, then it may take you right back to what happened when you were a child.
In terms of remembering the blanks, it’s imperative you do this in a place where you are psychologically “held” (safe), because remembering “requires you to feel the pain of what happened and grieve for what you lost”, says Stubley. If you are able to do some work to address the fallout it may help you feel that you have more choices about what kind of life you now want, and that you’re not stuck in this awful trauma.
There are some links below, but start with your GP. Surgeries vary hugely, but are a good place to start looking for some therapeutic help.
When the Body Says No — Caring for ourselves while caring for others. Dr. Gabor Maté
The Long Term Effects of Bullying
https://www.mentalhelp.net/abuse/long-term-effects-of-bullying/
You know how jokes are often funny because they are based in an ugly truth? I had a new realization of that phenomena while watching Bill Maher’s new stand-up comedy special “The Decider” on HBO the other night. Bill was talking about various recent sexual abuse scandals and was comparing the complaints made against Michael Jackson to complaints made against various Catholic priests with the aim of suggesting that what Michael allegedly did to his victims was gentle compared to the treatment received by victims of the priests. Seemingly out of nowhere, he started talking about a time when he was a child and was rather viciously beaten up during an incident of playground bullying. As part of his punchline, he commented that he would have gladly subjected himself to the worst abuse Michael has been accused of perpetrating rather than having to endure that single beating.
The comment resonated with me, probably because like Bill, I too was bullied as a kid, and also found the experience to be pretty ugly. I don’t think I’d ever choose to subject myself to Michael’s ministrations in order to have escaped my own bullying experiences (you gotta have standards in life), but I know I would have given a lot to have been able to stop them from happening.
The bullying I was subjected to did not occur on the playground, but rather on the school bus. I can vividly recall days when I would have to launch myself out of the school bus door and run as fast as I could up the hill to the shelter of my house. A group of older neighborhood boys would be after me for reasons that were never entirely clear. I was younger, more sensitive, certainly more vulnerable and not talented at fist fighting. Most days I’d make it home safely , but some days I’d end up belly up on the grass trying to fend off blows and kicks while a ring of kids jeered and cheered that day’s aggressor. A blow to the head and you’d see stars like in the cartoons.
I’m 40 years old now; it’s been something like 30 years since that sort of thing last happened. Still, the experience has not left me, it sucked so much. I don’t think about it much these days, but I know that having lived through those experiences has shaped me as an adult, and not for the better.
The experience of getting your face smashed in by bullies (or taunted by them, or pushed, or shoved, or excluded, etc. ) has got to be an almost universal sort of thing; something that many others who have endured similar experiences can perhaps recognize and respond to. In this spirit, I offer my self-disclosure (and hijack Bill’s) as seed for discussion.
There are lots of programs designed to help schools and other institutions prevent bullying. It’s kind of a hot topic these days in a small sort of way. Hopefully the things that researchers have and will come up will help limit the scope of the problem in the future. However, I’m quite confident that it will never go away entirely. It seems to me that bullying is just one of those things that are just a part of human nature. Something that can be suppressed but not eliminated.
Where I want to go with this essay is not to talk about how to make bullying stop, but rather, to explore the sorts of damage bullies do to their victims, and to discuss a few paths through which some of that damage can be, at least in part, undone.
Bullying is Abuse
Here’s a few statements to get us started: 1) Bullying is a form of abuse, and 2) Bullying is a narcissistic sort of act. In making the first statement here, I mean to say that both bullying and traditional forms of abuse are selfish and/or sadistic, destructive, and often violent acts perpetrated upon victims who do not in any way, shape or form deserve to be treated in that manner. In making the second statement I’m suggesting that ring-leader bullies (those who organize bullying) are behaving as though the emotional and physical health of their victims is not important or is at least less important than their own desire for the thrill of aggression and dominance. Narcissists treat other people as though they were objects either to be used, or discarded, and the bully both uses his victim (for purposes of self-gratification and aggrandizement) and then discards him.
Now, children are fairly narcissistic by their very nature. Children are not born appreciating that other people are actually just like they are with their own needs and independent rights. A long period of development must occur before children grasp that the other people around them have needs and interests just like they do and need to be accommodated and accorded respect. The golden rule of treating others as you would yourself like to be treated makes no sense to a young child who has not yet matured to the point where this basic appreciation of the individuality of every person has been grasped. Instead, children need to be held in line with what amount to incentives (and sometimes punishments) for acting as though other people matter. So by saying that bullying is a narcissistic action, I’m not at all saying that all bullies are narcissists. Adult bullies who have not outgrown their childhood narcissism probably do qualify, but little kids are just going to be that way. This is why I’m not terribly optimistic that we can solve the problem of bullying in our time.
Bullying Causes Long-Term Emotional Damage
The experience of being bullied can end up causing lasting damage to victims. This is both self-evident, and also supported by an increasing body of research. It is not necessary to be physically harmed in order to suffer lasting harm. Words and gestures are quite enough. In fact, the old saying, “Sticks and stones may break my bones but names will never harm me” is more or less exactly backwards. For the most part, physical damage sustained in a fist fight heals readily, especially damage that is sustained during the resilient childhood years. What is far more difficult to mend is the primary wound that bullying victims suffer which is damage to their self-concepts; to their identities. Bullying is an attempt to instill fear and self-loathing. Being the repetitive target of bullying damages your ability to view yourself as a desirable, capable and effective individual.
There are two ugly outcomes that stem from learning to view yourself as a less than desirable, incapable individual. The first ugly outcome is that it becomes more likely that you will become increasingly susceptible to becoming depressed and/or angry and/or bitter. Being bullied teaches you that you are undesirable, that you are not safe in the world, and (when it is dished out by forces that are physically superior to yourself) that you are relatively powerless to defend yourself. When you are forced, again and again, to contemplate your relative lack of control over the bullying process, you are being set up for Learned Helplessness (e.g., where you come to believe that you can’t do anything to change your ugly situation even if that isn’t true), which in turn sets you up for hopelessness and depression.
At the same time, you may be learning that you are helpless and hopeless, you are also learning how you are seen by bullies, which is to say, you are learning that you are seen by others as weak, pathetic, and a loser. And, by virtue of the way that identity tends to work, you are being set up to believe that these things the bullies are saying about you are true.
It would be great if the average person was possessed of unshakable self-confidence, but this just isn’t how identity works. Identity is a social process. Other people contribute to it. Particularly when people are young and have not yet survived a few of life’s trials, it is difficult for people to know who they are and what they are made of. Much of what passes for identity in the young (and in the older too) is actually a kind of other-confidence, which is to say that many people’s self-confidence is continually shored up by those around them telling them in both overt and subtle ways that they are good, worthy people. This is one of the reasons people like to belong to groups – it helps them to feel good about themselves. Bullying teaches people that they are explicitly not part of groups; that they are outcasts and outsiders. It is hard to doubt the reality of being an outcast and an outsider when you have been beaten or otherwise publicly humiliated. It takes an exceptionally confident (or otherwise well-supported) person to not internalize bullies’ negative messages and begin bullying yourself by holding yourself to the same standards that bullies are applying to you and finding yourself a failure. In other words, it is rather easy for bullying victims to note that they have been beaten up and then to start thinking of themselves as weak, no-good, worthless, pathetic, and incompetent. These are the sorts of thoughts that lead to depression, or, if they are combined with revenge fantasies, to anger and rage feelings.
Where the first ugly outcome of bullying unfolds rather immediately in the form of a wounded self-concept, the second ugly outcome unfolds more slowly over time. Having a wounded self-concept makes it harder for you to believe in yourself, and when you have difficulty believing in yourself, you will tend to have a harder time persevering through difficult situations and challenging circumstances. Deficits in academic performance can easily occur when bullying victims succumb to depression or otherwise become demoralized. They certainly also occur when victims ditch school to avoid bullies. The deficits themselves are not the real issue. The real issue is that if deficits occur for too long or become too pronounced, the affected children can lose out on opportunities for advancement and further study, and ultimately, employment. I’ve read retrospective studies where people report having left school early so as to avoid continued bullying, and this of course will have altered and limited the job prospects they have available to them as adults. Leaving school may be a dramatic (if occasionally realistic) example of how early bullying can affect one’s life, but there are surely other ways that anger or depression caused by bullying harms and developmentally delays people’s progress.
Inevitably, it is the sensitive kids who get singled out for teasing; the kids who cry easily; the easy targets. Targeted as they are, many sensitive kids learn to think of their sensitivity as a bad thing and to avoid it, and/or channel it into revenge fantasy and anger. This doesn’t much work when you are a kid (it is difficult to reinvent yourself without actually moving to a new place), and it can have negative consequences in adulthood when the same children, now emotionally avoidant or angry or cynical adults, find themselves having difficulty entering into or maintaining loving and warm intimate relationships.
A similar form of damage comes when bullied kids internalize negative attitudes concerning aspects of themselves that set them apart from others, such as their sexual orientation, minority group membership, or religious affiliation. In such cases, bullying sets up a peer pressure to reject aspects of one’s self which are fundamentally not rejectable, and thus a potentially lifelong tension gets set up inside that person. If anyone out there has a better idea for how someone can end up become a homosexual-hating homosexual, or a jew-hating jewish person or other seemingly self-contradictory person I’d like to know about it.
The following list, culled from my reading on this subject, summarizes some of the effects bullying victims may experience:
In the short term:
- Anger
- Depression
- Anxious avoidance of settings in which bullying may occur.
- Greater incidence of illness
- Lower grades than non-bullied peers
- Suicidal thoughts and feelings (In one British retrospective bullying experiences survey I came across (of unknown scientific value), 20% of the sample attempted suicide secondary to having been bullied, whereas only 3% of participants who were not bullied attempted suicide).
In the long term:
- Reduced occupational opportunities
- Lingering feelings of anger and bitterness, desire for revenge.
- Difficulty trusting people
- Interpersonal difficulties, including fear and avoidance of new social situations
- Increased tendency to be a loner
- Perception of self as easy to victimize, overly sensitive, and thin-skinned
- Self-esteem problems (don’t think well of self)
- Increased incidence of continued bullying and victimization
A few interesting observations of factors that seem to lessen the negative impact that bullying has on people have come to my attention during the process of cataloging the ways that bullying can mess you up. For instance:
Perception of Control
A 2004 Spanish college student sample study suggests that there is a direct relationship between victim’s perception of control over their bullying experience and the extent of long term difficulties they experience as a result of bullying. This is to say, that bullied students who believed they were able to influence and/or escape their bullies reported fewer negative long term effects from having been bullied than did students who felt helpless to influence their situation while it was happening. Perception of control (and not reality of control) was key in this study, as no relationship was found between the various ways that students coped with being bullied and how they turned out.
I can see the outline of a mechanism working here (where students who believed they still had control over their situations avoided developing learned helplessness and therefore had less of a chance of experiencing depression). However the study doesn’t really help us to know what to recommend that people do to lessen their chances of long term problems. Remember, it didn’t matter what the students actually did; it only mattered what they believed.
If we go with the idea that believing you have control over events is important then the thing to do if you are being bullied is to keep persevering in your efforts to stop the bullying as though those efforts will result in your being able to get the bullying to stop. No single thing you do may actually stop the bullying from happening, but the effect of continually working under the assumption that you haven’t tried all options and may still get the bullying to stop may do the trick. And, of course, you might actually get the bullying to stop because of something you do or don’t do.
Rather than try to control the past (which is impossible), it might make more sense for hurting victims to get themselves to focus on what they can control in the present, for the benefit of their future happiness and fulfillment. As the poet George Herbert’s classic phrase wisely advises us, “living well is the best revenge”.
Early Exposure
The age at which kids are first bullied seems to be important according to some research. Young children who are first bullied during their pre-teen years appear to be less negatively impacted in the long term than are children who are first bullied as teens. People first bullied as young children report experiencing higher long-term stress levels than do people who were never bullied. However, people who were first bullied as teens report more long term social withdrawal and more reactivity to violence than other groups. There is a greater tendency towards the use of self-destructive coping mechanisms in the first-bullied-as-teens group, and an interesting but hard to make sense of sex difference, where women tend to become more aggressive as a result of their bullying experience, and men to demonstrate a greater tendency to abuse substances. I can’t help but wonder if the increased independence and emancipation that teens enjoy makes them more likely to experiment with and then get locked into maladaptive coping strategies like substance abuse than their younger peers.
Social Support
Finally, multiple researchers point to the protective effect that a good social support network has with regard to bully victim’s short and long term outcomes. Having supportive family members and peers around who can be confided in when one has been bullied and who can offer support and advice tends to lessen bullying’s impact.
There are a number of reasons why it makes sense that a supportive social network should help, but one of them deserves to be made explicit. Namely, that when a bullying victim is surrounded by and bought into a supportive social network, they are receiving many positive messages about their worth from network members, and there are thus fewer opportunities for bullies’ negative messages to find purchase and grow to take over self-esteem. If bullies can only succeed in harming people physically; if they do not succeed in harming them emotionally or harming their identities, then relatively little lasting damage can be done.
Undoing the Damage
If the primary damage that bullying causes is damage to identity and self-esteem, then taking steps to repair identity and self-esteem are in order for people looking to heal from past bullying experiences. What needs to heal, in most cases, is not the physical body, but rather, identity and self-concept. Bullied people need to learn how to feel safe again in the world (or safe enough). They need to learn that they are acceptable people who have something to offer other people. They need to feel in more control over their moods and urges. They need to feel again that if they set their mind to something that they can hope to accomplish it. These are not modest goals, by any chance, but they are the sorts of things that bullying victims need to think about working on.
I’ll refer people to our topic centers on Depression and Anger Management for ideas about how these problems can be treated. Cognitive Behavioral Therapy is likely to be of particular utility with regard to depression and anger that is secondary to having been bullied because mood problems that have originated in this way are very likely to have come into being as a result of victims having become convinced that they are worthless and incompetent. In the language of cognitive behavioral therapy, these would be thought of as dysfunctional core beliefs which could be addressed and repudiated using cognitive restructuring techniques that encourage people to closely examine such beliefs and dispute them when they are found to contain exaggerations and distortions (which these sorts of beliefs surely will).
Social withdrawal problems and social anxiety also can be very profitably addressed within the context of cognitive therapy. One of the really nice things about a therapy setting is that role playing can take place between therapist and patient so as to provide anxious patients with opportunity to practice and improve how they will interact in feared but desired social situations. When basic social fears and skill deficits have been addressed, it should become easier for socially withdrawn people to find the connections they need to finally feel fundamentally accepted by others.
I typically hate the overused word “empowered”, but I’m going to use it here, because it really fits here. People who have been bullied have been fundamentally dis-empowered. Their feelings of personal safety have been violated and their belief in their own competency and adequacy has been brought into question. Such people may exist in a state of perpetual avoidance and paralysis. In order to feel good about themselves, they will need to break through that paralysis and engage in something that helps them feel like they are gaining in power. Not power over others, but power over themselves. No other people can do this for them. Each paralyzed person has to decide to empower themselves.
There are a million avenues one can go in to fulfill an empowerment goal, the one that is right for any given person being a function of that person’s talents and opportunities. Anger can be productively funneled into a competitive endeavor (such as education, business, sports, gaming or some other means of becoming excellent) or a creative expression. Fears can be faced down and courage can be found. I, as author of this essay, cannot offer specifics on how this can be accomplished as the right path for each person will be individual, but I can say that it is more or less as simple as picking out a goal you desire to accomplish (which will assert yourself) and then deciding to make it happen. As with any self-improvement goal, it is good to start small, and to dissect larger goals into their smallest possible elements, so that each step you take on the way to a big goal is manageable. You can read more about this process in our Psychological Self-Tools self-help book.
I’ll end here with an appeal for comments and contributions. Have I missed anything important with regard to being bullied, in your opinion and experience? What are your own experiences with having been bullied? How has bullying shaped your life, for better or for worse? What are the problems that you developed as a result of having been bullied, and how have you managed to address them? What messages can you give to young people who are being bullied today. What would you have done differently if you could do it over? The more people who contribute to this essay, the more useful of a resource it can become.
Do our eyes hold the secret to treating some mental illness? Ottawa researchers tout unique psychotherapy | Ottawa Citizen
An unconventional eye-movement therapy that can treat everything from chronic pain to PTSD is pushing the boundaries of psychotherapy in unexpected directions. Andrew Duffy reports on the growing number of therapists and researchers in Ottawa and beyond using EMDR.

Article content
When he first read about a new psychotherapy that used eye movement to help alleviate patients’ trauma, psychologist Philippe Gauvreau was deeply skeptical.
The field was beset by pseudoscientific fads, and he was convinced Eye Movement Desensitization and Reprocessing (EMDR) was just another one. The therapy combines exposure therapy with guided eye movements: Typically, a patient is asked to track a therapist’s hand while thinking about a traumatic event.
Proponents insisted EMDR could change the way difficult memories were stored in the brain, making them easier to manage for those with post-traumatic stress.
“Like many, many, many psychologists, I went, ‘What is this BS?’ This is a bunch of hooey,” remembers Gauvreau, a practitioner in the Outaouais.
He became so exercised by EMDR’s entry into the field of psychotherapy that he resolved to train in the technique so he could more knowledgably dismantle it as a treatment. In October 2000, he enrolled in an EMDR course in Ottawa – and changed his mind.
Article content
“I just fell in love with the approach,” he says.
For the past 20 years, Gauvreau has employed EMDR in hospitals and at his private practice in Maniwaki. He has qualified as an EMDR trainer, led more than 30 training sessions, chaired Canada’s annual conference for EMDR, and researched EMDR’s ability to treat anxiety.
He’s now among a growing number of therapists and researchers exploring EMDR’s use on everything from chronic pain to depression to addiction. EMDR has also inspired new eye-involved treatments – variants such as Brainspotting, Flash Technique and EMDR 2.0 – that are pushing the frontiers of psychotherapy in new directions.

“In psychiatry, we had been focused for so long in the mind that we’d forgotten the body,” says University of Ottawa psychiatry professor Dr. Jeanne Talbot, who also holds a doctorate in neuroscience.
EMDR and its offshoots ask clients to be aware of what’s going on in their bodies at the same time that they’re thinking about a traumatic incident. Talbot, who has trained in Brainspotting, has seen clients experience pronounced physical reactions during treatment sessions.
“We have to be cautious because we’re all burned out psychiatrists and this is a difficult field, but when it works, Brainspotting is like psychodynamic therapy on speed,” she says, referring to a more traditional and holistic psychotherapy.
Finding an effective treatment for trauma is a central pursuit of psychotherapy research since unresolved trauma is at the root of so many mental illnesses and addictions. “That stuff from the past we haven’t been able to get over, that stuff feeds our current situation,” says Gauvreau.
EMDR is the brainchild of Brooklyn-born psychologist Dr. Francine Shapiro, who conceived of the therapy while on a walk in May 1987. She had gone to a San Francisco Bay area park, and was dwelling on a traumatic memory from her own past — she had recently overcome breast cancer — as she darted her eyes left and right to take in the scene. For some reason, her unease lifted.
“I wanted to see if it would work if it was deliberate,” she once recalled, “so I brought up something that bothered me, moved my eyes in the same way, and saw the same thing happening.”
She later found that her eyes moved rapidly back and forth, spontaneously, whenever a disturbing thought came to mind. “The thoughts disappeared,” Shapiro wrote in her book on the subject, “and when I brought them back to mind, their negative charge was greatly reduced.”
She enlisted friends to try it and discovered that eye movements alone did not ease the pain of troubling memories. So she developed a treatment that evolved into the eight-phase program now known as EMDR. In its key phase, Shapiro had clients bring a traumatic event to mind while tracking her fingers as she moved them left and right for 20 to 30 seconds.
The first scientific studies of EMDR were published in 1989, and in the three decades since then, more than 30 randomized controlled trials have confirmed it as an effective treatment for PTSD. Those studies have found that EMDR can significantly reduce PTSD symptoms.
“What is effective in EMDR is not new, and what is new is not effective,” Harvard University psychologist Richard McNally wrote in 1999.
Others criticized proponents for outracing the science with zealous marketing. “EMDR provides an excellent vehicle for illustrating the differences between scientific and pseudoscientific therapeutic techniques,” University of New England psychologist James D. Herbert declaimed in the Clinical Psychology Review.
In succeeding years, however, scientific evidence mounted in support of EMDR’s effectiveness. Therapists reported breakthroughs with PTSD in relatively short periods of time. Its popularity spread.
In 2013, the World Health Organization endorsed it alongside cognitive behavioural therapy (CBT) as an advanced treatment for PTSD. Four years later, the U.S. Department of Veterans Affairs recommended it as a first-line treatment for PTSD. The International Society for Traumatic Stress Studies followed suit.
In 2017, the American Psychiatric Association conditionally recommended EMDR for the treatment of PTSD, but gave a stronger rating to CBT and prolonged exposure therapy. (The advisory panel, however, acknowledged its recommendation could change based on new evidence.)
Before the therapy, a clinician will evaluate a client, offer some self-calming techniques, and identify a distressing memory along with the negativity that goes with it. For example, if someone was in a serious car crash, the individual might say something like, “I don’t feel safe.” The therapist will offer an alternative idea to replace it such as, “I’m a survivor.”
In the critical “desensitization” phase — the only one that involves eye movement — a client is asked to concentrate on the traumatic memory and its negative consequences while following the therapist’s hand as it moves back and forth across their field of vision. (Sometimes, a moving light or object is used to induce eye movement. In her research with blind patients, Shapiro found that hand taps and noises could produce similarly effective “bilateral stimulation.”)

Dr. Andrew Burr, a clinical psychologist at The Ottawa Anxiety and Trauma Clinic, says he uses EMDR for a wide range of trauma-related issues, including child abuse, sexual assault, bullying, infidelity and divorce. He studied the approach after hearing colleagues talk about its ability to reach “a new level of healing.”
“Once I started using EMDR,” he says, “I found that I could see my clients experiencing, live in session, changes to the way they felt about memories that had long upset them.”
“There is almost a sense of disbelief at times when the client feels calmer and less bothered by an issue — and can’t really explain what changed except that it feels different,” says Burr, who holds a PhD in clinical psychology.
Clinical social worker Anne Bailliu has been using EMDR to treat traumatized former soldiers and RCMP officers since 2009 at The Royal’s Operational Stress Injury Clinic.
Bailliu says she assesses each client to understand what therapy might work best for them. Soldiers, she says, tend to respond well to prolonged exposure therapy since it’s better known and more structured than EMDR.
“EMDR can sound airy-fairy to them,” she says.

In her experience, Bailliu says, the therapy works best with clients who have a repressed memory or one that they’re reluctant to talk about. “EMDR is a method to be able to access disturbing or upsetting memories that are unresolved,” she says. “But the person doesn’t have to talk about them, so for some clients that’s very appealing.”
The therapy can produce strong physical and emotional reactions: “It can be quite cathartic for some people,” she says.
Why does it work? That question remains an intriguing mystery. EMDR’s inventor, the late Dr. Francine Shapiro, theorized that the therapy took advantage of the same mechanisms involved in rapid eye movement (REM) sleep. Research has shown that REM sleep is important to the healthy consolidation of memories.
Until recently, researchers could only guess at what was actually going on inside the brain during EMDR. Then, in 2019, a study published in the leading scientific journal Nature offered the first potential clues as to EMDR’s biological underpinnings.
In that study, scientists in South Korea repeatedly exposed mice to a sound that was paired with an electric shock to establish a disturbing memory that connected the two. They then exposed one set of mice to the same sound with no shock, and at the same time, to a light that oscillated in front of them. The other set of mice were exposed to the sound without the shock or the moving light.
Researchers found that the mice exposed to the moving light – it was designed to mimic EMDR therapy – exhibited a “clear and persistent” decrease in their fear responses: They were less likely to freeze when they heard the sound again.
The scientists then explored what was happening in the neural circuits of the animals’ brains. They found that the moving light stimulated connections between brain regions in the mice thought to be responsible for sensory processing, and dampened activity in another part of the brain that encodes fear.
The success of EMDR has inspired a number of spinoffs, including Brainspotting, a technique with a large Ottawa following.
Three uOttawa assistant professors have been qualified to teach Brainspotting, which requires clients to identify a point in their visual field, a brainspot, where a memory or emotion is particularly vivid. Two of those psychiatrists, Dr. Jane Evans and Dr. Marjorie Robb, have trained 325 mental health workers in the Ottawa region, including more than 25 psychiatrists, during the past three years.
“The most unlikely psychiatrists are coming and asking, ‘What is this?’” says Prof. Jeanne Talbot, who is also trained to teach Brainspotting but is concentrating her efforts on research. She contends Ottawa may have more therapists trained in Brainspotting than any other city in the world.

Dr. Talbot was deeply skeptical when first introduced to Brainspotting by her friend, Dr. Evans. She talked about it so much that one night, at a bar, Talbot demanded to see the therapy in action. Her friend invited Talbot to think about something that was deeply upsetting, so Talbot thought about the recent election of U.S. president Donald Trump.
“In my chest,” Talbot told her.
Evans then pulled out a pointer and brought it across her friend’s visual field. She told Talbot to note any change.
“Wouldn’t you know it, she pulls it across to the right part of my visual field and the feeling in my chest goes up,” Talbot remembers. Her eyes flickered at the same time.
Talbot was intrigued. Six weeks later, she enrolled in a training course in Connecticut and was astonished to find everyone else in the course had a similar experience when they practised Brainspotting on each other. Many in the class complained of Trump-related trauma.
“We were doing a lot of Trumpspotting,” Talbot says. “So I came back to Ottawa thinking, ‘What the hell was that?’”
She tested Brainspotting with a few willing patients in her private practice. Many of them found it helpful, Talbot says, and ended up asking her, “What the hell was that?”
One client, a traumatized refugee, told her that every refugee who seeks treatment should have the chance to try it. “It was enough to get me interested, for sure,” she says.
Talbot is now working to produce data to establish Brainspotting’s efficacy and investigate its impact on the brain’s neural networks. Talbot wants to use an EEG and a specialized MRI to better understand what’s happening inside the brain during the therapy.
One theory holds that Brainspotting exerts a similar effect on the brain as mindfulness meditation, which helps to regulate emotions.
Talbot says Brainspotting and other EMDR-inspired psychotherapies hold tremendous potential, but she warns that building scientific evidence in support of them will take time: “There’s the possibility of a true paradigm shift in what traditional medicine has to offer individuals with trauma, but it’s slow process.”
How to Leave Your Comfort Zone and Enter Your ‘Growth Zone’
https://positivepsychology.com/comfort-zone/
 Life is full of opportunities to step outside the comfort zone, but grabbing hold of them can be difficult.
Life is full of opportunities to step outside the comfort zone, but grabbing hold of them can be difficult.
Sometimes the problem is not being aware of reasons to do so. After all, if the feeling of comfort signifies our most basic needs are being met, why should we seek to abandon it?
What holds people back most of the time is their frame of mind rather than any distinct lack of knowledge.
This article looks at the shifts in thinking required to step outside of comfort and into personal growth. Along the way, we’ll outline useful tools, tactics, and examples to help make leaving the comfort zone as rewarding as possible.
Before you continue, we thought you might like to download our three Goal Achievement Exercises for free. These detailed, science-based exercises will help you or your clients create actionable goals and master techniques to create lasting behavior change.
This article contains:
What Is the Comfort Zone in Psychology?
Now firmly embedded in cultural discourse, the metaphor of ‘leaving one’s comfort zone’ became popular in the 1990s. The phrase ‘comfort zone’ was coined by management thinker Judith Bardwick in her 1991 work Danger in the Comfort Zone:
“The comfort zone is a behavioral state within which a person operates in an anxiety-neutral condition, using a limited set of behaviors to deliver a steady level of performance, usually without a sense of risk.”
Within the comfort zone, there isn’t much incentive for people to reach new heights of performance. It’s here that people go about routines devoid of risk, causing their progress to plateau.
But the concept can be traced further back to the world of behavioral psychology.
In 1907, Robert Yerkes and John Dodson conducted one of the first experiments that illuminated a link between anxiety and performance.
They saw that mice became more motivated to complete mazes when given electric shocks of increasing intensity – but only up to a point. Above a certain threshold, they began to hide rather than perform.
Corresponding behavior has been seen in human beings. This makes sense because in response to anxiety-provoking stimuli, the options are either fight (meet the challenge), flight (run away/hide), or freeze (become paralyzed).
The Yerkes–Dodson Law (Yerkes & Dodson, 1907) is true not just for more tangible types of performance, such as being given a stressful new task at work, but also in many life areas such as understanding ourselves, relating to others, and so on.
The core idea is that our nervous systems have a Goldilocks zone of arousal. Too little, and you remain in the comfort zone, where boredom sets in. But too much, and you enter the ‘panic’ zone, which also stalls progress:
From Comfort Zone to the Growth Zone
When leaving the comfort zone, fear doesn’t always equate to being in the panic zone. As the below diagram shows, fear can be a necessary step en route to the learning and growth zones:
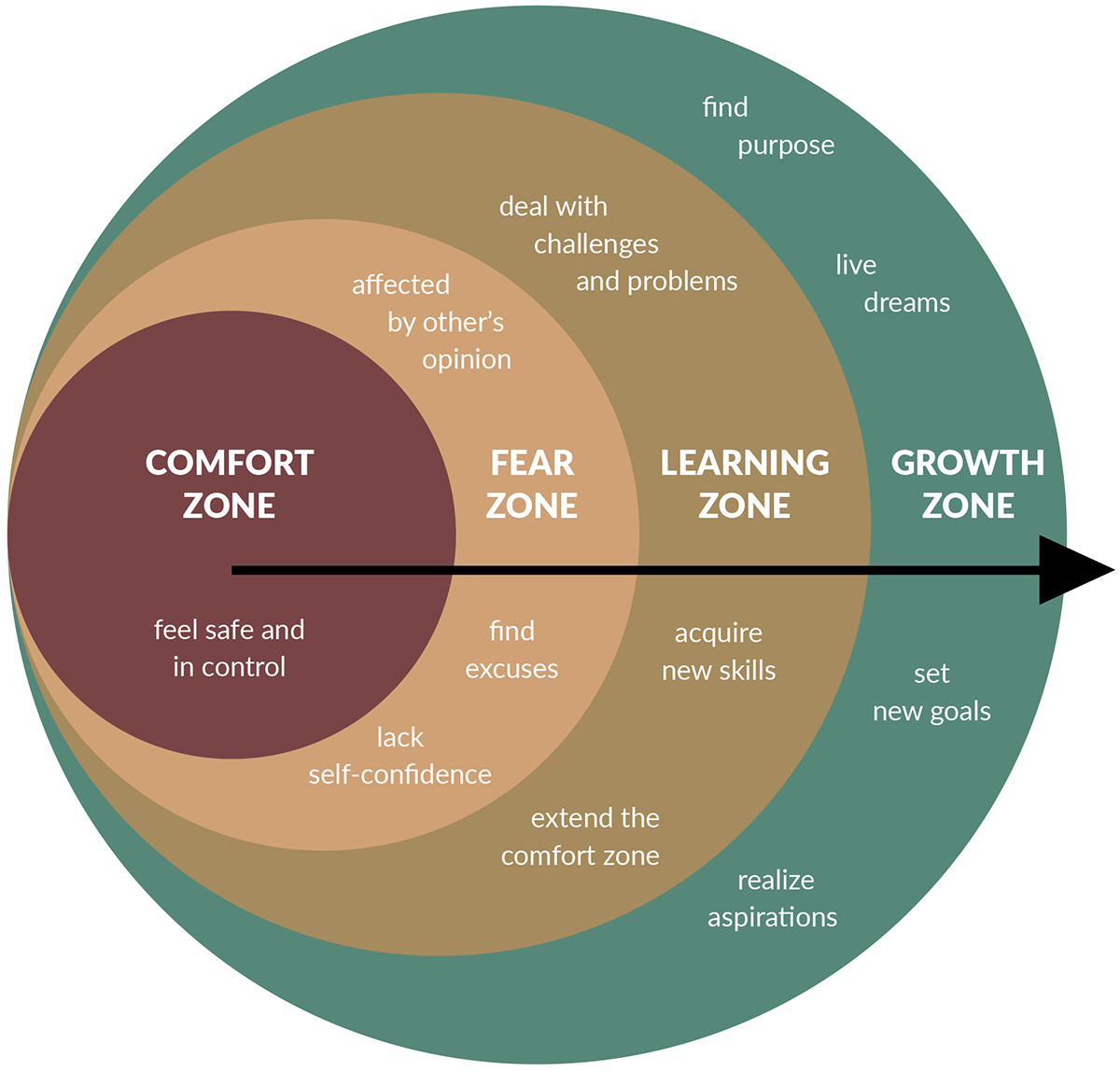
Source: PositivePsychology.com ‘Leaving The Comfort Zone’ Toolkit
It takes courage to step from the comfort zone into the fear zone. Without a clear roadmap, there’s no way to build on previous experiences. This can be anxiety provoking. Yet persevere long enough, and you enter the learning zone, where you gain new skills and deal with challenges resourcefully.
After a learning period, a new comfort zone is created, expanding one’s ability to reach even greater heights. This is what it means to be in the growth zone.
It’s important to state that like most behavioral change attempts, moving into the growth zone becomes harder without some level of self-awareness. Thus, it can be beneficial for clients to consider the following:
- How big are their zones?
Across every life domain, everyone’s zones vary in size. To leave your comfort zone, you must appreciate its outer limits. Similarly, you must develop an intuitive sense of where your panic zone lies. Taking on challenges that lie somewhere in between will stretch you, leading to growth and learning. - What are their strengths?
Understanding and capitalizing on personal strengths can be of great use. Most people have experience leaving the comfort zone in at least one area of life, and there are usually plenty of insights to be uncovered from this experience.
In reality, the process of moving from the comfort zone to a growth zone may not be linear. Peaks, troughs, and plateaus often complicate the journey. Sometimes, we even need to retreat to the comfort zone periodically before mustering the strength to leave again. Nevertheless, appreciating the steps can help in tolerating uncertainty.
While occupying the comfort zone, it’s tempting to feel safe, in control, and that the environment is on an even keel. It’s smooth sailing.
The best sailors, however, aren’t born in smooth waters.
We’ll explore a few powerful benefits of leaving the comfort zone in the next section.
Benefits of Leaving the Comfort Zone: 4 Examples
Aside from enhancing performance, there are plenty of less-direct benefits of leaving the comfort zone. A full list would require a separate article, so here are four top-line, broadly applicable examples.
1. Self-actualization
For many, self-actualization acts as a powerful incentive to leave the comfort zone. The concept was popularized through Abraham Maslow’s (1943) theory of human motivation, which he described as follows: “What a man can be, he must be. This need we may call self-actualization.”
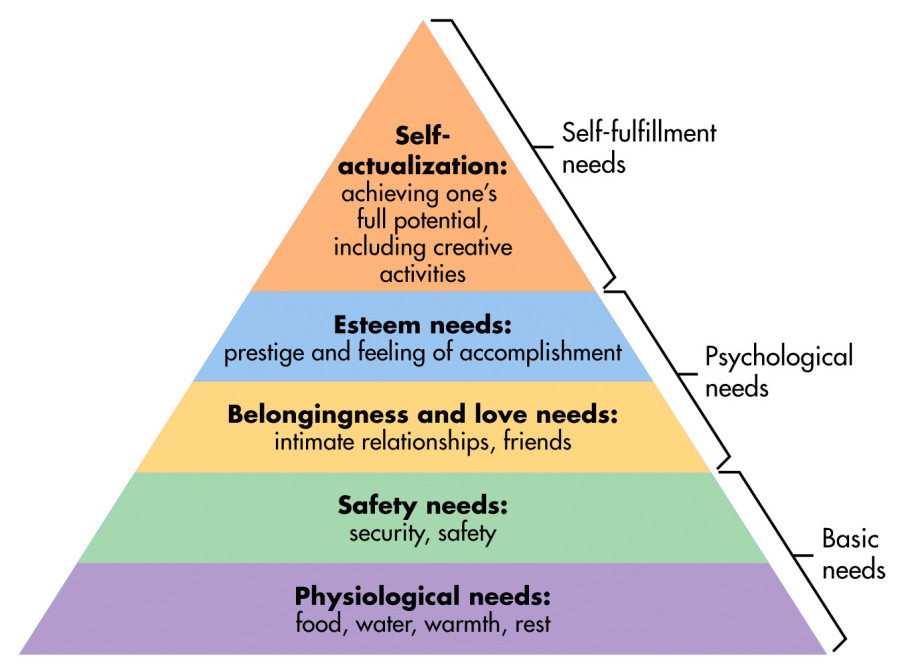
Maslow’s hierarchy of needs operates like a ladder, with the satisfaction of our ‘basic’ and ‘psychological’ needs being analogous to inhabiting the comfort zone. But whether we’re conscious of it or not, the theory argues our next requirement is for personal growth and fulfillment.
As long as the decision to leave the comfort zone aligns with a person’s values, this shift is akin to making a bid for self-actualization. Why is this important? For one, not striving for growth could mean falling into a state of inertia later in life.
2. Development of a growth mindset
Stanford psychologist Carol Dweck’s (2008) work on mindsets marked a paradigm shift in the field of positive psychology. Her research distinguished between two contrasting belief systems – the fixed versus growth mindsets.
With a fixed mindset, people believe they have set doses of each ability, with a corresponding ceiling on how much they can achieve. Failure reveals inadequacy, and criticism becomes a fatal blow to self-esteem.
The growth mindset means recognizing humans as malleable. From this stance, setbacks become opportunities for learning (Dweck, 1999) and our potential becomes unlimited.
Intentionally leaving the comfort zone goes hand-in-hand with developing a growth mindset. While the fixed mindset keeps us trapped by fear of failure, the growth mindset expands the possible. It inspires us to learn and take healthy risks, leading to positive outcomes across life domains.
3. Resilience and antifragility
Life isn’t exactly a predictable affair; perhaps then, people shouldn’t be either. Sooner or later, everyone faces adversity. A habit of expanding our comfort zone equips people to handle change and ambiguity with more poise, leading to resilience.
Taking this further, statistician Nassim Taleb (2012) introduced the concept of ‘antifragile’ systems, which “thrive and grow when exposed to volatility, randomness, disorder, and stressors.” Examples include evolution and immune systems, as well as the human psyche.
While resilient systems bounce back to the same level after a shock, antifragile systems learn to grow from them, reaching new heights. To step outside the comfort zone then is to purposefully cultivate antifragility – so long as we don’t veer into the panic zone!
4. Greater self-efficacy
As outlined by Albert Bandura (1997), self-efficacy is the belief in being able to execute necessary actions in service of a goal. Goals that lead to higher self-efficacy are specific, not too difficult, and short-term (Yailagh, Lloyd, & Walsh, 2009).
Leaving the comfort zone means a phase of trial and error, during which at least some level of success is inevitable. Experiencing this success builds our self-efficacy, with belief in our ability starting to grow.
Like other benefits of leaving the comfort zone, this probably won’t happen overnight. Yet the cumulative upward spiral of achievement and confidence can become a potent asset for anyone.
4 Tips to Support Leaving Your Comfort Zone
What follows are four useful tips to support clients in leaving their comfort zones. These are a mix of mindset tips and practical guidance on setting goals.
1. Reframe stress
Physiologically, there’s no difference between anxiety and excitement (Smith, Bradley, & Lang, 2005). Both entail a ‘stress response,’ but whether they’re perceived as positive or negative is a matter of labeling.
Society tends to conceptualize all stress as ‘bad,’ but the idea of ‘eustress’ or ‘positive stress’ challenges this. Eustress provides the energy to get through a public speech, go on a romantic date, and so on. These stimuli can be reframed as exciting, propelling us out of the comfort zone.
2. Understand neuroplasticity
An essential step toward internalizing the growth mindset is to embrace neuroplasticity research. Once understood, less courage is needed to make the first move away from comfort because failure itself becomes integral to the journey.
At the core of Dweck’s theory is that humans are malleable and adaptable. Another good way to appreciate her philosophy is by watching this TED talk:
3. Prioritize
Occupying the comfort zone isn’t always detrimental. For example, it might be reasonable to stay in your ukulele-playing comfort zone but not your managing-personal-finances one.
The point is to identify bottlenecks: areas of life where being too comfortable does more harm than good. Encourage goal selectivity in clients so they can focus effectively.
4. Small steps
It’s okay to take small, methodical steps, as well as larger, bolder ones. Leaving behind the comfort zone doesn’t mean recklessly throwing caution to the wind. Every step forward is progress.
Patiently fostering self-awareness while intelligently assessing each zone’s boundaries is a sure way to make the process as smooth as possible.
7 Ways to Leave Your Comfort Zone
Having covered the what, why, and how of leaving your comfort zone, let’s now cover seven ways someone might try to do so.
1. Do everyday things differently.
In everyday life, there are ample opportunities to challenge yourself. Turn off your smartphone and television while having dinner, decide what to wear more quickly, or just slow down to take in the surroundings on a walk. These changes break you out of old, comfortable routines.
2. Expand your professional skillset.
Growing your skillset can foster creativity and refresh your self-confidence, as well as increase employability. Skills like public speaking, negotiation, and leadership can represent a new challenge for many people. Investing in them can build resilience, personal satisfaction, and open up more opportunities than ever.
3. Try a new diet.
Many people want to improve their diets and stop relying on ‘comfort foods.’ Doing so often means trying something new.
Sticking to a healthy diet can be as challenging as it is rewarding, with self-efficecy growing as you hit milestone goals along the way.
4. Take workouts to the next level.
Similarly, many aspire to this goal. For some, it can mean running their first 5K, but for others, it might be completing a triathlon.
Aiming high with exercise is emblematic of leaving the comfort zone and a great way to get the ball rolling.
5. Get creative.
Creativity – anything from writing a poem to building a business – usually involves an element of risk. Creative endeavors are about stepping into the unknown, with failing and subsequent learning as expected outcomes.
Exercising creativity is a good way to train yourself to have a growth mindset and let go of a need for perfection from the outset.
6. Challenge your beliefs.
While exploring alternative perspectives can be uncomfortable, it enables growth and insight by challenging entrenched beliefs.
This might take several forms, such as reading varied book genres, diversifying who you talk to, and visiting new places. It’s easy to get stuck in our ways, but this can lead to complacency – a hallmark of being in the comfort zone.
7. Practice honesty.
When employed sensitively, honesty can be a tremendous catalyst for personal growth. Whether being straight with yourself in a private journal or telling someone close how you feel, honesty forces people out of their comfort zone. Through honest communication, we can understand ourselves better and build deeper bonds with others.
10 Inspiring Quotes
Here are ten quotes that encapsulate many of the ideas discussed:
All growth starts at the end of your comfort zone.
Tony Robbins
You can only grow if you are willing to feel awkward and uncomfortable when you try something new.
Brian Tracy
My comfort zone is like a little bubble around me, and I’ve pushed it in different directions and made it bigger and bigger until these objectives that seemed totally crazy eventually fall within the realm of the possible.
Alex Honnold
Do one thing every day that scares you.
Eleanor Roosevelt
Becoming is better than being. The fixed mindset does not allow people the luxury of becoming. They have to already be.
Carol Dweck
One can choose to go back toward safety or forward toward growth. Growth must be chosen again and again; fear must be overcome again and again.
Abraham Maslow
Without continual growth and progress, such words as improvement, achievement, and success have no meaning.
Benjamin Franklin
You have calibrated life when most of what you fear has the titillating prospect of adventure.
Nassim Taleb
The level of effort you tolerate from yourself will define your life.
Tom Bilyeu
May your choices reflect your hopes, not your fears.
Nelson Mandela
PositivePsychology.com’s Useful Tools
PositivePsychology.com is an excellent repository of tools you can leverage in supporting clients to leave their comfort zones behind.
Our Toolkit offers various worksheets and exercises designed to help people enter the growth zone and realize their potential.
Here are three examples:
- Facing the Effect of Fear-Based Beliefs on Goal Achievement
This tool introduces clients to the impact of fear-based beliefs on goals and personal growth. Exercises challenge them to analyze how their anxieties stop them from pursuing goals that would be meaningful to them. - Leaving the Comfort Zone
This tool helps clients weigh the costs of staying in the comfort zone. The four zones are explored in more detail, with questions to prompt clients to apply the knowledge to their own lives. Ultimately, the goal is to trigger a positive upward spiral of personal fulfillment. - Moving Toward a Growth Mindset
This intervention moves people toward the growth mindset by correcting fixed mindset thoughts. The exercise encourages active reflection, with a useful ‘mindset log’ worksheet.
An additional resource that may seem bizarre yet revealing is titled My Gravestone. For any client reluctant to depart from a comfortable routine, reflecting on their future tombstone could be a remarkable incentive to step into a growth mindset.
A Take-Home Message
Recognizing opportunities to leave the comfort zone isn’t always easy; neither is seizing them with conviction.
It’s crucial to cultivate a mindset that lays strong foundations, paving the way toward the growth zone. This includes seeing yourself as inherently adaptable, reframing stress, and believing in your ability to endure fears and doubts.
Every person faces this choice, knowingly or not. You can settle for what you know – the seemingly safe, familiar, and routine. Or, you can become receptive to opportunities for growth, challenging your personal status quo and seeing what you’re capable of.
When this becomes a habit, the benefits to be reaped throughout life are copious. Not only are disappointments curbed and regrets avoided, but we also reach our highest human potential, acting as an inspiration to others.
We hope you enjoyed reading this article. Don’t forget to download our three Goal Achievement Exercises for free.
If you’d like to help others succeed in life, our Motivation & Goal Achievement Masterclass© is a comprehensive training template for practitioners that contains everything you need to help your clients reach their goals and master motivation-enhancing techniques.
The Long Term Effects of Childhood Trauma | Kati Morton
Effects of Childhood PTSD: Crappy Childhood Fairy
Creating a Calm Place: Grounding Activity for Anxiety
Grounding Activities are an essential skill for managing Anxiety, Stress, PTSD, and improving mental health. Visualizing a Safe place can be an essential technique for grounding the body and mind. When stress, anxiety, or panic seem to be taking over, we can actually trigger our nervous system to respond by calming the body and mind through “perceived safety”. By bringing to mind your safe space, your favorite environment, or your comfort zone you can actually reverse the stress response. This is an essential coping skill for managing anxiety, panic, and PTSD. Do you feel stressed out even when nothing’s the matter? Do you feel tense, anxious or panicky? Our amazing brain has the ability to imagine danger in a way that triggers that fight flight freeze response, even when we’re safe. But we can counteract that “danger” response by bringing to mind a safe place.














8 Comments. Leave new
June 18, 2020 12:41 am
Thanks heaps . I think the line between emotional only and what happens when child gets older ie flash back with physical recall will be blurred. Maybe care givers/parents can inflict trama by response to aberant activity between children. What you say to them for such behavior will be taken quite literally. in emotion age recall stage. They probably have issues relating to knowledge beyond years. Such as all the phycological stuff to come from gaining such exparances.
June 22, 2020 11:30 am
Thanks for your comments. We’re pleased to hear our blog post resonated with you. Children can take parents’ comments literally, and what they take on board can hang around and reappear as flashbacks when they’re older. If you’re experiencing them yourself, and they’re becoming an issue for you, then do reach out for professional support.
September 3, 2020 4:58 am
I’ve recently been DX with C-PTSD from long term domestic violence. How do emotional flashbacks take place for this vs the C-PTSD emotional flashbacks for childhood trauma. The latter seems to be the norm that is mostly discussed therefore must be more common for C-PTSD. Do you have an article addressing this side of C-PTSD and emotional flashbacks? Thanks.
September 8, 2020 8:32 am
Hello. Thanks for taking time to read our blog and post your comments. Flashbacks can be incredibly intense and distressing, making you feel you’re right back at the original horrifying event. We’re sorry to hear you’ve been through long-term domestic violence. We haven’t yet created an article that looks at flashbacks and domestic violence, but we will do so in response to your request.
October 16, 2020 10:23 am
Hi it only happens now and then so 3yrs ago my son slammed his bedroom door shut and took my daughters finger off it was horrible but every now and then I see it all again happening it comes back a lot when I see the fire fighters frist responder drive past me or if its parked I see it all and then just cry, how can I stop it and it probley sounds silly.
October 26, 2020 3:05 pm
Hi Michelle. This does not sound silly at all. Flashbacks can happen when we haven’t processed an emotional experience that was overwhelming at the time. You may want to reach out for support with a therapist who works with flashbacks and traumatic experiences. Your GP may be a good place to start. Wishing you all the best.
October 20, 2020 10:59 pm
I found myself nodding yes a lot while reading this article. I am now dealing with the memories of my childhood popping up here and there. Strange that I didn’t realize it before. Thank you
October 26, 2020 3:01 pm
Hello Brian. We’re pleased to hear that our blog post has been useful for you. Being able to identify when you’re having an emotional flashback can give you more time and choice as to how to deal with it. Wishing you well.